Summary
Splenic tuberculosis (TB) is an uncommon extrapulmonary manifestation, typically observed in immunocompromised individuals, but can also occur in immunocompetent patients1.We report a 45-year-old immunocompetent male who presented with prolonged fever. Imaging revealed multiple hypodense splenic lesions, and histopathology confirmed Mycobacterium tuberculosis infection. The patient was treated with standard anti-tuberculosis therapy (ATT), resulting in complete clinical and radiological resolution. This case highlights the importance of considering splenic TB in the differential diagnosis of fever of unknown origin (FUO), especially in endemic areas, and underscores the effectiveness of medical management alone in selected cases2.
Introduction
Splenic involvement in tuberculosis is rare and is usually seen in miliary or disseminated TB, especially among HIV-positive or otherwise imunocompromised patients3. Isolated splenic tuberculosis in immunocompetent individuals is uncommon and often presents with non-specific symptoms such as fever, weight loss, and abdominal discomfort 4. Radiologically, splenic TB may mimic pyogenic abscess, lymphoma, or fungal infections, making diagnosis challenging without histopathological confirmation 5. High clinical suspicion, especially in endemic regions, and prompt initiation of Anti-TB can result in successful outcomes without the need for surgical intervention 6.
Case report
45-year-old previously healthy man from Yangon, admitted to Tropical and Infectious Diseases Department on December 2024 with chief complaint of fever for 3 weeks. Regarding system review, no positive symptom except loss of weight, appetite and left-sided abdomen discomfort. On examination, only mild anemia detected. Investigations revealed anaemia with ESR 98, CRP 79 with normal liver and renal functions. No vegetation on echocardiogram, infectious serology all negative, blood and fungal cultures were sterile. ( Table 1). CXR was normal but on USG (abd) multiple splenic abscess were detected. CT(abd) was proceeded and it stated multiple splenic SOL likely micro-abscesses with hepatosplenomegaly. To differentiate splenic lymphoma, fungal infection or tuberculosis, splenic biopsy was done and histopathology report revealed chronic granulomatous inflammation composed of fibroblasts, lymphocytes, plasma cells, and Langhans giant cells with necrotic debris. These findings were highly suggestive of tuberculous aetiology in the appropriate clinical and radiological context. Fungal elements and malignant cells were not identified. (fig.2) He was diagnosed as extra-pulmonary TB and started anti tuberculous medications (4FDC) according to body weight. After anti TB, wellbeing improved with resolving fever over 2 weeks. Recheck CT (abd) after 2 months of anti TB showed resolving splenic abscesses. After 3 weeks of hospitalization, he was discharged and advised to attend infectious diseases clinic at YGH on follow-up. And He was put on anti TB for 1 year duration because some residual splenic abscess were found on recheck CT (abd) after 6 months of anti TB. 7
Table(1) Results of Investigations
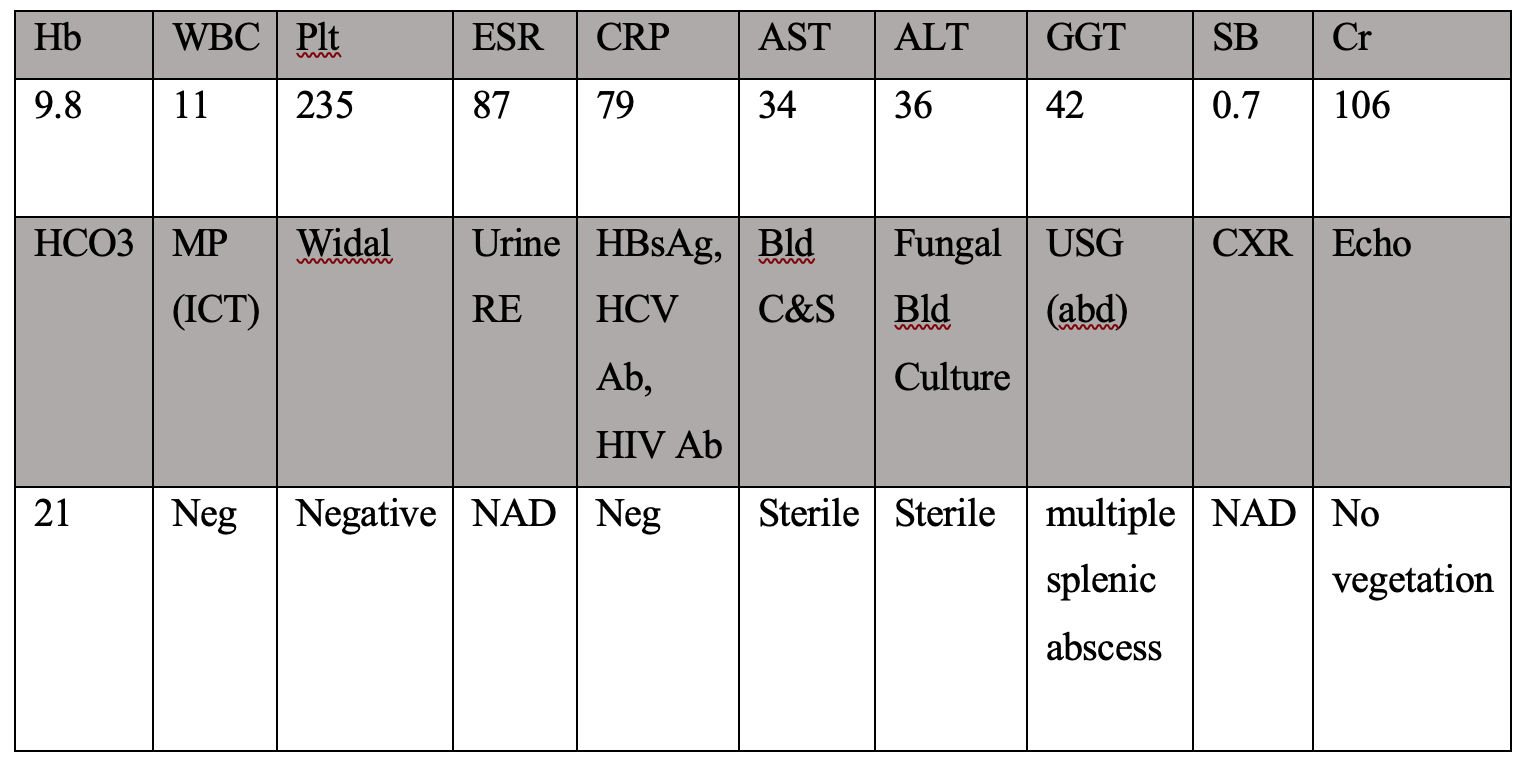
Table (1) Investigations of patient
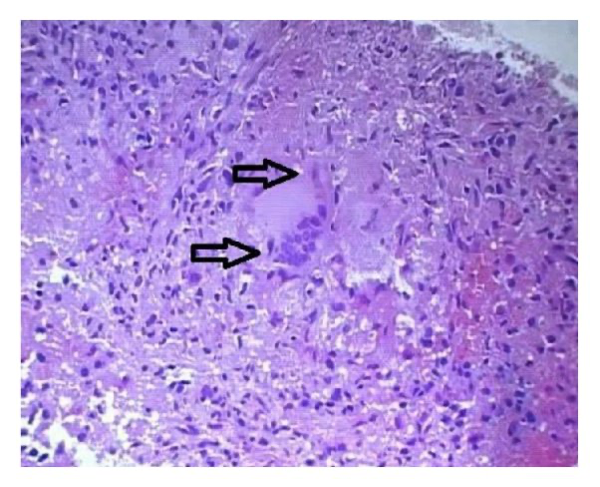
Fig 2. Histopathology of splenic biopsy of patient
Discussion
Tuberculosis remains a major public health concern, particularly in endemic countries like Myanmar 8. Extrapulmonary tuberculosis accounts for about 15–20% of all TB cases, with abdominal TB representing approximately 11% of extrapulmonary cases 9. Splenic tuberculosis can occur either as part of miliary TB or as an isolated organ involvement, the latter being extremely rare in immunocompetent hosts 10. In our patient, CT imaging showed multiple hypodense splenic lesions, a finding consistent with tuberculous abscesses 11. Histopathological examination revealing granulomatous inflammation with caseation necrosis confirmed the diagnosis of splenic TB 12. The resolution of symptoms and radiologic improvement following standard Anti-TB supports medical therapy as an effective treatment option 13. Unlike pyogenic splenic abscesses which may require drainage, tubercular abscesses usually respond well to Anti-TB alone 14. A high index of suspicion and timely biopsy or aspiration for diagnosis can help avoid unnecessary surgical interventions like splenectomy 15. Our case underscores the importance of considering TB in patients with FUO and splenic lesions, particularly in TB-endemic regions 16.
Conclusion
Isolated splenic tuberculosis should be considered in patients presenting with prolonged fever and splenic lesions, even in the absence of immunosuppression 17. CT imaging and histopathological confirmation are critical for accurate diagnosis 18. Prompt initiation of Anti-TB can lead to full clinical and radiological resolution, often without the need for surgical intervention 19. In TB-endemic settings, early recognition and appropriate therapy can prevent complications and reduce morbidity 20.
References
- Sharma SK, Mohan A. Extrapulmonary tuberculosis. Indian J Med Res. (2004);120(4):316–353.
- Huang DB, Kunesh M, Rishi M. Isolated tuberculous splenic abscess. J Infect. (2001);42(2):147–149.
- Lee JY. Diagnosis and treatment of extrapulmonary tuberculosis. Tuberc Respir Dis (Seoul). (2015);78(2):47–55.
- Chien RN, Lin PY, Liaw YF. Isolated splenic tuberculosis in an immunocompetent patient. J Clin Gastroenterol. (1992);15(1):88–90.
- Chong VH. Splenic tuberculosis: a rare entity. South Med J. (2007);100(6):635–638.
- Dasgupta A, Singh N, Bhatia A. Abdominal tuberculosis: a histopathological study with special reference to intestinal perforation and mesenteric vasculopathy. J Lab Physicians. (2009);1(2):56–61.
- Hamizah, R., Rohana, A.G., Anwar, S.A., Ong, T.Z., Hamzaini, A.H. and Zulkarnaen, A.N., (2007). Splenic tuberculosis presenting as pyrexia of unknown origin. The Medical journal of Malaysia, 62(1), pp.70-71.
- WHO. Global Tuberculosis Report 2023. World Health Organization.
- Bhargava DK, et al. Abdominal tuberculosis in India: an overview. Int J Tuberc Lung Dis. (1998);2(8):569–577.
- Grover S, Puri T, Sharma S. Isolated splenic tuberculosis in an immunocompetent patient. Trop Gastroenterol. (2011);32(3):219–221.
- Kim SH, et al. Imaging of tuberculous peritonitis and its mimics. Radiographics. (2001);21(3):559–569.
- Andronikou S, et al. Splenic tuberculosis in children: radiologic-pathologic correlation. Pediatr Radiol. (2002);32(1):16–23.
- Rathi P, Gambhire P. Abdominal tuberculosis. J Assoc Physicians India. 2016;64(2):38–47.
- Lin WR, et al. Isolated splenic tuberculosis mimicking splenic abscess: a case report. World J Gastroenterol. (2006);12(9):1545–1547.
- Das CJ, et al. Imaging diagnosis of tuberculosis in the abdomen. Postgrad Med J. (2007);83(986):389–397.
- Nzegwu MA, et al. Isolated splenic tuberculosis presenting as fever of unknown origin. Afr Health Sci. (2013);13(2):451–453.
- Maharaj B, Leary WP. Isolated tuberculous abscess of the spleen. S Afr Med J. (1981);60(5):179–180.
- Ooi LL, Leong SS. Splenic abscesses from 1987 to 1995. Am J Surg. (1997);174(1):87–93.
- Kapoor VK. Abdominal tuberculosis. Postgrad Med J. (1998);74(874):459–467.
- Sharma MP, Bhatia V. Abdominal tuberculosis. Indian J Med Res. (2004);120(4):305–315.
Author Information
Aye Mya Theingi Win, Khin Rupar Ko, Aye Aye Win , May Zabe, Nyunt Thein
- Senior Consultant physician, Tropical and Infectious Diseases Department, Yangon General Hospital
- Professor, Tropical and Infectious Diseases Department, Yangon General Hospital
- Associated Professor, Tropical and Infectious Diseases Department, University of Medicine (1), Yangon
- Senior Consultant physician, Tropical and Infectious Diseases Department, Yangon General Hospital
- Senior Consultant physician, Former Head of Department of Medicine, Emeritus Professor of Medicine, University of Medicine (1), Yangon