It is better to comply with the international guidelines and current trends.
OSA (obstructive sleep apnea syndrome) has become a worldwide health problem effecting millions. This is a sleep-related breathing disorder with breathing-related night-time symptoms as a sequel to sleep-related day-time symptoms. It also complicates comorbid cardiopulmonary and metabolic disorders. Polysomnogram (sleep test) is the gold standard diagnostic procedure according to ICSD3, 2014(TR)1 manual.
Nasal CPAP is the main treatment for adult OSA patients recommended by AASM2.
In day-to-day clinical practice, we are seeing OSA patients who came with sleep test results. Thus why, making decision to treat an adult OSA patient by CPAP or different modalities becomes an academic challenge. Let’s see AASM clinical practice guidelines for OSA treatment with CPAP (2019)3
AASM recommendation No.1- we recommended that clinicians use PAP compared to no therapy to treat OSA in in adults with excessive day time sleepiness. (Strong).
Yes, it is true after identifying 38 RCTs3 that assessed the efficacy of PAP to treat excessive daytime sleepiness. Currently OSA treatment tends to be individualized based on phenotypic classification.
Under anatomical and pathophysiological differences among OSA patients, 4 phenotypes 4 were classified among current literatures as upper airway collapsibility, high loop gain (ventilation instability), poor upper airway dilator muscle function and low EEG arousal threshold.
There were definitely CPAP responsive group of OSA patients known after many clinical trials5.Among the OSA sufferers, obese young adult male with abnormal day time sleepiness being the most CPAP responsive group5 (see the figure1).
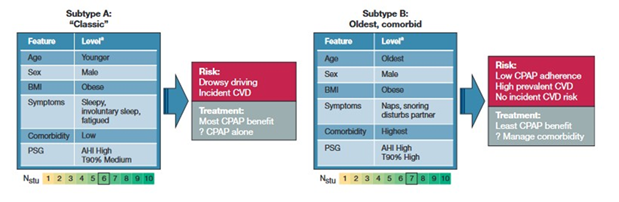
Fig 1. Sub type of OSA patients with different CPAP responses from American College of Chest Physician, chest.2019.09.002.
In contrast, elderly patients with underlying multiple comorbidities were the poorest responsive group5. In this group, control of underlying comorbidity and treatment with OA (Oral Appliances) or MAD (Mandibular Advancement Device) will be better than CPAP.
Other treatment modalities such as drug therapy, O2 therapy and corrective surgery are also recommended according to phenotypes and underlying pathophysiology (individualized).
Currently, CPAP adherence is defined as nightly usage of minimal 4 hr for at least 5 to 7 nights per week6 and some organizations such as health insurances count >4 hr for 70% of the nights.
To normalize day time sleepiness, minimal 4 hr per night is enough known after most studies, but for truck drivers at least 6 hr per night usage is required for normal level of alertness and 7.5 hr is required to get normal daytime functions6. This showed dose response relationship to get good treatment outcome.
We also need to aware of poor CPAP adherence among OSA patients. According to many clinical trials, non-adherence rates were estimated up to 50% (range; 29 to 83%) depending on study types6.
The clinical predictors, that influence on the poor CPAP adherence6.
1- Patients with very high AHI and BMI.
2- Patient with poor intuition about personal health.
3- Upper airway anatomical problems.
4- Patient with insomnia
5- OSA patient with no day time sleepiness.
On the other hands, CPAP associated new onset insomnia (NOI) was detected up to 21.1% of OSA patients found in clinical studies7 which also effect CPAP adherence.
Recent studies also pointed circuit (PAP tubing) depended CO2 retention in OSA patients especially in APAP users related to poor PAP adherence and day time symptoms8.
What should we do for CPAP adherence by the OSA patients?
AASM recommendation No.7; We recommended that educational interventions be given with initiation of PAP therapy in adult with OSA (Strong)3.
Close monitoring when starting CPAP therapy
Make a time to talk with OSA patients to know benefit and side effects of PAP therapy and advice how to deal with the treatment problems. PAP device supplier role is also important to help OSA patient with device setting adjustment for successful OSA therapy. This is a team work and all persons concerned must be work together for the patient to get successful therapy. Early detection of PAP related problem and timely problem solving by the team are the most important factors. Regular and close follow up either by face to face or online consultations within few weeks of therapy are very essential for patient’s trust on PAP treatment.
“Right choice of CPAP masks”
Mask choice is another important factor for patient’s compliance. According to studies, nasal masks are considered better than oronasal type due to low pressure requirement and more adherence by the patients9 (see figure2). Humidifying function in PAP also prevents nasal congestion and dry mouth, common complaints by PAP users.
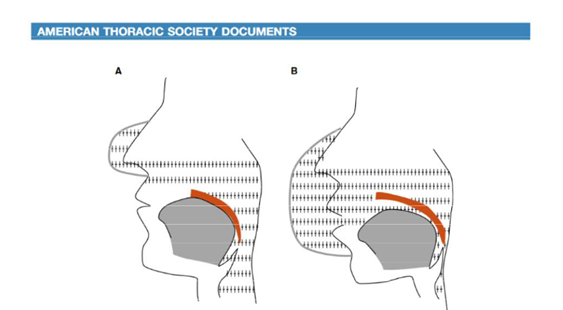
Fig. 2 Potential effect of oronasal continuous positive airway pressure (CPAP) on upper airway patency. (A) Nasal CPAP splints the upper airway and pushes the soft palate against the tongue.(B) Oronasal CPAP may neutralize the splinting effect of nasal CPAP because of the transmission of positive pressure to the mouth (from Ann Am Thorac .Soc Vol 17, No.10 ,Oct 2020).
Treat the comorbidities overlapping with OSA
We should also look for underlying insomnia, nocturnal on set of pain, comorbid sleep disorders other than OSA, drugs which disturb normal sleep including hormones, mood disorders, substance abuse, oronasal anatomical and obesity related problems; all should be addressed with care.
AASM recommendation No.4; We recommended positive airway pressure therapy be initiated using either APAP at home or in lab pap titration in adult with OSA and no significant comorbidities (Strong)3.
Selecting the mode of CPAP
CPAP is a respiratory assist device (RAD) which splint upper airway to prevent collapse during sleep by using a therapeutic air pressure measure by cm H2O ranging from 4 to 20 cmH2O and recommending CPAP to right group of OSA patients will achieve successfully OSA treatment.
Traditionally, prescription of CPAP to OSA patients was fixed CPAP pressure, manually determined after in lab titration either by split night or full night titration study.
APAP (auto pressure pap) does not need in lab titration, thanks to the technology and also convenient for patients who needs urgent attention. But, APAP is not recommended to OSA patients with underlying significant cardiopulmonary and neurological diseases because all PAP studies excluded these underlying conditions3.
Do we always check nocturnal hypoxia correction during CPAP treatment?
We must also check nocturnal hypoxia in some patients that CPAP alone cannot solve the problem. In OSA patients overlapping with COPD, interstitial lung diseases, CHF, obesity hypoventilation syndrome and severe post Covid lung fibrosis, for whom additional O2 supply with titrated flow rate is required together with CPAP to correct nocturnal hypoxia. During this procedure we must ensure proper admixture of additional O2 concentration and flow rate upon underlying PAP device for successful therapy.
Treatment for adult OSA patients without day time sleepiness is still a big challenge.
CPAP usage did not demonstrate clear benefit on cardiovascular morbidity and motility due to poor design among clinical trials3.
Task force members from AASM explained that “there is insufficient and inconclusive evidence to either recommend or withhold PAP to treat non –sleepy adult with OSA as a means to reduce cardiovascular events or mortality”3.
In these patients, conservative management of OSA, with monitoring for development of OSA symptoms over time, may be appropriate3.
Finally, OSA in adult patient is considered as chronic disease with trending towards personalized therapy. Although CPAP is the main treatment option for most adult OSA patients, clinician should aware of current guidelines and trends to deal with different groups of OSA patients with different clinical settings.
Care should be patient centered and team work approach by all persons concerned to achieve successful OSA therapy for patients who actually required CPAP.
References
1. ICSD, international classification of sleep disorders and diagnostic manual, published in year 2014, Text Revision.
2. AASM; American Academy of Sleep Medicine
3. Treatment of adult obstructive sleep apnea with positive airway pressure; An American Academy of Sleep Medicine clinical practice guidelines 2019,journal of clinical sleep medicine vol.15, No.2
4. Phenotype of obstructive sleep apnea and Direct targeted therapy, Current Respiratory Medicine Review, 2020, Vol.16, No. 2 77
5. Phenotypic sub type of OSA, A Challenge and Opportunity for Precision Medicine,157-2 chest Feb 2020.
6. Assessing and managing non adherence with continuous positive airway pressure for adults with obstructive sleep apnea; Uptodate.com; Feb 28, 2024,
7. Int. J. Environ. Res. Public Health 2021, 18, 9248
8. Circuit-dependent Co2 rebreathing during continuous positive airway pressure; sleep medicine, Vol, 121. September 2024, page 42-47.
9. Treatment of adult obstructive sleep apnea with positive airway pressure an AASM systemic review, meta- analysis and GRADE assessment; Susheel P. Patil.journal of clinical sleep medicine.Vol.15. No.2
Author Information
Zay Ya Aye
M.B., B.S, M.Med. Sc, Internal Medicine.