Adult Dengue Infection
Abstract
Dengue infection has been ranked as the most important mosquito-borne viral disease with epidemic potential because about half of the world’s population is now at risk1.Moreover, there is a change in epidemiology of dengue in South East Asia countries and shift in affected age groups is evident2. Also in reviewing medical records from Yangon General Hospital, adult dengue patients are increasing year by year3. Since specific antiviral treatment and effective vaccine have not developed yet, adult dengue infection becomes an alarming impact on human health and national economy. So it is very essential to for the clinicians to know more about this disease to diagnose disease in early stage to achieve good outcome.
Epidemiology
In Myanmar, all four serotypes are circulating with increasing possibility of genetic mutation. First dengue outbreak occurred in Yangon in 1964 and outbreaks have occurred in 3-5 year cycles until 2000 but more frequent thereafter4.According to report from VBDC, dengue cases increase from 1654 in 1970 to 24178 in 2019 in which more and more adult patients are involved5.
Immunopathogenesis
Antibody dependent enhancement mechanism, complement are all contributing factor resulting in “Cytokine Tsunami” which in turn lead to vascular permeability6. Children have a higher susceptibility to plasma leakage than adults and DSS was less frequent in adult dengue patients7. But multiorgan failure like expanded dengue syndrome is more common in adult patients. Therefore it is seem that there is little different in immunopathogenesis between paediatric and adult patients.
Dengue serotypes
In treating dengue patient, clinician should be aware of prevailing dengue types in the country. Because there are serotype specific clinical manifestations, laboratory parameters and severity of diseases 8.In Myanmar, prevailing dengue serotype changes from time to time and according to the study done at Yangon General Hospital, most prevalent serotype was DEN-3 followed by DEN-1 and DEN-4in 20199.
Clinical course and manifestations of dengue infection
1. Febrile phase
This acute febrile phase usually lasts 2−7 days and most of adult dengue patients present with myalgia, arthralgia and nausea whereas pediatric patients usually present with vomiting and skin rash10. It can be difficult to distinguish dengue clinically from non-dengue febrile diseases in this phase. But progressive decrease in total white cell count should alert the physician to a high probability of dengue virus infection6.
2 Critical phase
This phase usually occurs on days 3–8 of illness with transition from the febrile to afebrile phase. Persistent vomiting and severe abdominal pain are early indications of plasma leakage. Children have a higher susceptibility to plasma leakage than adults do. Therefore, DSS was less frequent in adult dengue patients7. But severe organ involvement, also known as expanded dengue syndrome like severe hepatitis, encephalitis, and myocarditis are more commonly found in adult patients6.
3. Recovery phase
Gradual reabsorption of extravascular compartment fluid takes place in this phase. Bradycardia and ECG changes are common findings during this stage. Respiratory distress from pulmonary oedema will occur if excessive intravenous fluids have been administered especially in patient with underlying cardiac problem6.
1. Diagnostic Tests
(i) Virological methods – RT-PCR, NS1 Ag
(ii) Serological methods – Ig M, Ig G (secondary infection is more common in adult patient than paediatric patient)11
2. Disease Monitoring Laboratory Tests
(i) Full Blood Count (FBC)-Leucopenia with rising HCT followed by progressive thrombocytopenia is suggestive of dengue infection. However, comparing adult and pediatric patients, high HCT and low platelet count are more common in adult patients. In recovery phase, the white blood cell count usually starts to rise soon after defervescence but the recovery of the platelet count is typically later than that of the white blood cell count10.
(ii) Liver Function Test- The frequency and degree of elevation of the liver enzymes are higher in DHF compared to DF11. Liver enzymes abnormality is more commonly seen in adult than pediatric patients10.
(iii) Laboratory investigations for patients who present with profound shock or no clinical improvement in spite of adequate volume replacement–A-Acidosis, B-Bleeding, C-Calcium, S-Blood sugar6.
Management of adult dengue infection
There is no direct antiviral therapy available against the DENVs. Management is supportive, which largely consists of maintaining adequate intravascular volume. Early detection of disease progression and access to proper medical care lowers fatality rates of severe dengue to <1%1.
1. Out-patient management (Group A)11
- Encourage oral intake of ORS, fruit juice and other fluids
- Give paracetamol for high fever
- Monitor warning signs daily by health care provider
2. In-hospital management ( Group B and C )11
(1) Non-shock patients (DHF Grade I & II)
- Encourage adequate oral fluid intake.
- IV fluid is indicated in patients who are vomiting or unable to tolerate oral fluids.
- Crystalloid is the fluid of choice for non-shock patients.
- Start with 5-7 ml/kg/hr for 1-2 hours, then reduce to 3-5 ml/kg/hr for 2-4 hrs and then reduce to 2-3 ml/kg/hr or less according to the clinical response.
(2) Dengue Shock Syndrome (DSS) (DHF Grade III & IV)
- Dengue shock syndrome is a medical emergency.
- All patients with dengue shock should be managed in high dependency / intensive care units. Fluid resuscitation must be initiated promptly. (figure 1)
(3) Blood transfusion in Dengue virus infection
- Patients with mild bleeding such as from the gums or per vagina, epistaxis and petechiae do not require blood transfusion.
- Platelet prophylaxis may be considered in adult dengue with underlying hypertension, heart disease, or those with anticoagulant or antiplatelet aggregation therapy and have marked thrombocytopenia <10,000 cells/cumm.
Discharge criteria11
- Absence of fever for 24 hours without the use of antipyretics, and a return of appetite
- Visible improvement in clinical picture
- Stable haematocrit
- Three days after recovery from shock
- Platelet count greater than 50,000/mm3 and rising
- No respiratory distress
- Resolved bleeding episodes
- Resolution/recovery of organ dysfunction
Vaccine against dengue infection
In 2019, US FDA approved CYD-TDV as first licensed vaccine but it can only be used in children of middle school and there is still not licensed vaccine for adult until now.
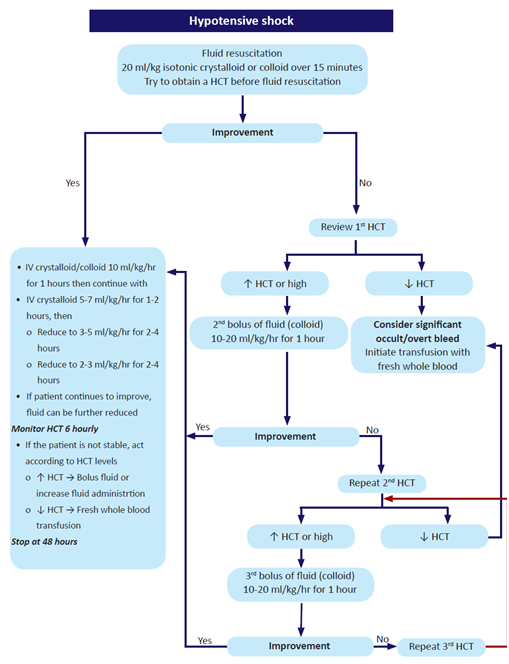
Figure 1 : Algorithm for management of hypotensive shock.
Conclusion
Dengue has emerged as a global life-threatening public health concern, affecting around 2.5 billion individuals in more than 100 countries. The physician should be aware about the varied and unusual clinical manifestations of this condition, changing trend of serotype, necessary blood tests and ensure a timely and adequate treatment plan. Future directions to combat this dreadful disease should aim at successful control of mosquito, development of vaccine, and antiviral drug.
References
- WHO (2020) Fact sheet on dengue and severe dengue
- Bhatia, R., Dash, A. P. and Sunyoto, T. (2013) Chainging epidemiology of dengue in South-East Asia.WHO South-East Asia journal of public health. 2(1), 23-27
- Annual Medical record of Yangon General Hospital ( 2018)
- Myat, T.W., Thu, H.M., Kyaw, Y.M., Aye, K.M., Win, M.M., Mar, W., Aye, K.S., Kyaw, T. and Thant, K.Z. (2016) Identification of dengue virus serotypes in children with dengue infection admitted to Yangon Children’s Hospital in 2014. Myanmar Health Sci Res J, 28(1), 60-64.. 28(1), 61-64.
- Ministry of Health and Sport Myanmar (2019) VBDC annual report.
- WHO (2011) World Health Organization. South East Asia Region. Comprehensive Guidelines for Prevention and Control of Dengue and Dengue Haemorrhagic Fever. Revised and expanded edition.
- Lum, L.C.S., Guzman, M.G., Martinez, K., Tan, L.H., Hung, N.T. (2012) Handbook for Clinical Management of Dengue. 2nd ed. Switzerland: WHO
- Halsey ES, Marks MA, Gotuzzo E, Fiestas V and Suarez L. (2012) Correlation of Serotype-Specific Dengue Virus Infection with Clinical Manifestations. PLoSNegl Trop Dis .6(5), 1-8.
- Aye-Mya-Theingi-Win(2019) Clinical manifestaions, laboratory parameters and sesverity of disease in adult dengue infection of different dengue serotypes. Dr.Med.Sc (tropical and infectious diseases) Thesis. University of Medicine 1, Yangon.
- WHO (2012) World Health Organization . Handbook for Clinical Management of dengue.
- Thanachartwet, V., Oer-Areemitr, N., Chamnanchanunt, S., Sahassananda, D., Jittmittraphap, A., Suwannakudt, P., Desakorn, V. and Wattanathum, A., 2015. Identification of clinical factors associated with severe dengue among Thai adults: a prospective study. BMC infectious diseases, 15(1), p.420.
- Ministry of Health and Sport Myanmar, (2018) National Guideline for Clinical Management of Dengue Version 01.
Aye-Mya-Theingi-Win1, Moe-Moe-San2
Consultant physician, Tropical and Infectious Diseases Department, Yangon General Hospital
Professor/Head, Tropical and Infectious Diseases Department, Yangon General Hospital