MANAGEMENT OF HYPERTENSION- CURRENT CONCEPTS
Hypertension is one of the strongest risk factors for almost all the different cardiovascular diseases 1. Despite the well tolerated and effective strategies for life style and drug treatment, control rate of hypertension remains poor globally and hypertension still remains as major preventable cause of cardiovascular diseases globally, driving 10 million deaths2. Worldwide, 1.4 billion peoples have hypertension among which less than 15% have blood pressure control to the target3.
DEFINITION AND CLASSIFICATION OF HYPERTENSION
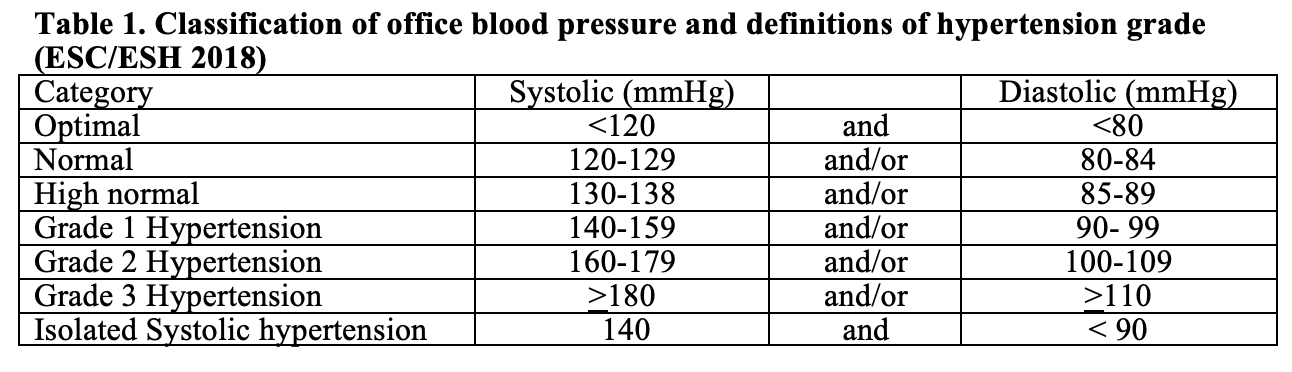
Hypertension is defined as the level of blood pressure (BP) at which the benefits of treatment unequivocally outweigh the risks of treatment, as documented by clinical trials. With the background of the outcomes of SPRINT (Systolic Blood Pressure Intervention Trial), ACC/AHA guidelines 2017 hypertension was redefined at lower level (130-139 mmHg systolic or 80-89 mmHg diastolic BP)4. ESC/ESH (2018) guidelines still defined hypertension as office systolic BP (SBP) values >140 mmHg and/or diastolic BP (DBP) values >90 mmHg. (Table 1).
AIM OF HYPERTENSION TREATMENT
Ultimate aim of the management of hypertension is to reduce the cardiovascular morbidity and mortality. Basing treatment decision on absolute cardiovascular risk combined with level of blood pressure is more cost-effective and able to save the more quality adjusted life-years3.
RISK STRATIFICATION (HYPERTENSION STAGING)
As the aim of antihypertensive treatment is to prevent the cardiovascular mortality, it is important to stratify the risk of CVD death in making decision for treatment threshold, treatment goal, defining the intensity of treatment and choice of treatment modality and medications. Factors including the risk stratification are stage of hypertension, CVD risk assessment score, hypertension mediated organ damage (HMOD) and presence of co-morbidities like diabetes and chronic kidney disease3. (Table 2)

Cardiovascular risk stratification
Stratification of cardiovascular risk of the individual is the important initial step in hypertension management. Different guidelines used the different method of CVD risk stratification. European guidelines use Systemic Coronary Risk Evaluation (SCORE) system5. Other useful systems of risk assessment are ASCVD risk calculator4 and WHO/ISH Cardiovascular Risk Prediction Chart6.
INITIATION OF ANTIHYPERTENSIVE TREATMENT (TREATMENT THRESHOLD)
In addition to the level of blood pressure (grade of hypertension), age of the individual, cardiovascular risk and presence of hypertension mediated target organ damage (HMOD) should be considered in making decision for the initiation of antihypertensive treatment including life style modification.
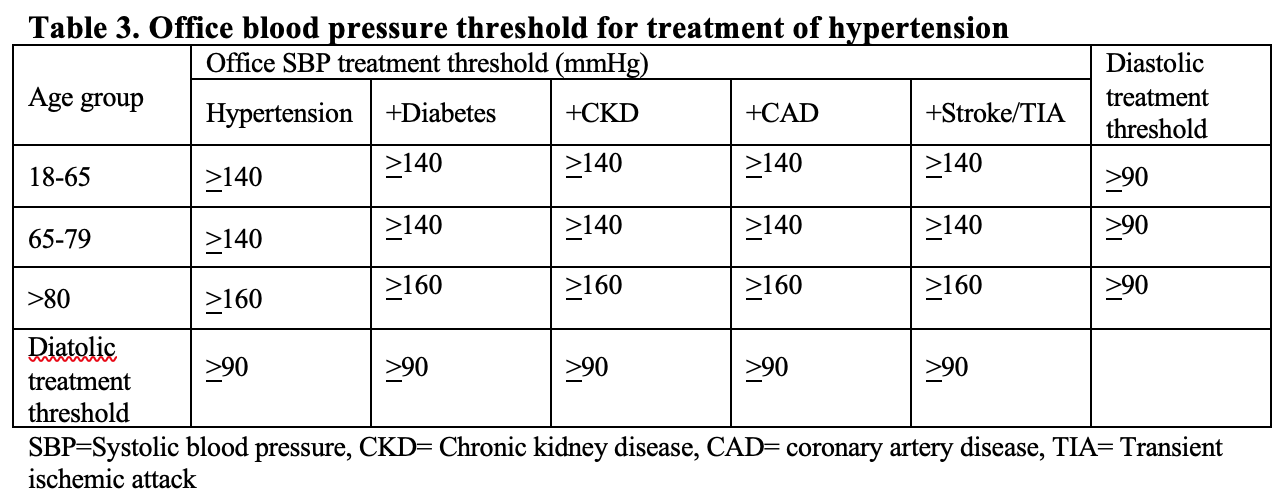
According to ESC/ESH 2018 , drug treatment may be considered even in the stage of high normal BP when CV risk is very high due to established CVD, especially coronary artery disease. In patients with grade 1 hypertension at low–moderate-risk and without evidence of HMOD, BP-lowering drug treatment is recommended if the patient remains hypertensive after a period of lifestyle intervention. BP-lowering drug treatment and lifestyle intervention is recommended in fit older patients (>65 years but not >80 years) when SBP is in the grade 1 range, provided that treatment is well tolerated. Recommendations for treatment threshold are summarized in following table. (Table 3)
BLOOD PRESSURE TREATMENT TARGETS
According to ESC/ESH 2018 guidelines, the first objective of treatment should be to lower the BP to <140/90 mmHg in all patients provided that the treatment is well tolerated, treated BP values should be targeted to 130/80 mmHg or lower in most patients. There is safety boundaries (ie. treated systolic BP not below 130 mm Hg in subjects aged 65 years or more, and not below 120 mm Hg in subjects aged less than 65 years ) is set in ESC/ESH 2018.
ACC/AHA 2017 guidelines recommended a target blood pressure of less than 130/80 mmHg adults with confirmed hypertension and known cardiovascular disease or 10-year atherosclerotic cardiovascular event risk of 10% or higher. Treatment target of less than 130/80 mmHg is also considered reasonable for the adults without additional markers of increased CVD risk.
LIFE STYLE CHANGES IN MANAGEMENT OF HYPERTENSION
Life style changes (non-pharmacological therapy) have important roles in hypertensive as well as non hypertensive individuals. In hypertensive patients including those with high normal BP, life style changes should be adopted as initial therapy or as adjunct to the drug therapy in all stages of treatment. It can facilitate drug step down or even drug withdrawal in highly motivated individuals who achieve and sustain the practice. It can also prevent or delay the onset of hypertension. It can be important beyond blood pressure control like reduction of cardiovascular death and prevention of cancer7.
Recommended life style changes in hypertensive patients are:
– Salt restriction to less than 5 grams per day
– Restricted alcohol consumption ( less than 14 units/week for men and less than 8 units/week for women)
– Avoidance of binge drinking
– Increased consumption of vegetables, fresh fruits, fish, nuts, unsaturated fatty acids (olive oil), low consumption of red meat, and consumption of low-fat dairy products.
– Body weight control to avoid obesity and to aim at healthy body mass index
– Regular aerobic exercise (e.g. at least 30 min of moderate dynamic exercise on 5–7 days per week)
– Smoking cessation and supportive care and referral to smoking cessation programs2
PHARMACOTHERAPY OF HYPERTENSION (ANTIHYPERTENSIVE AGENTS)
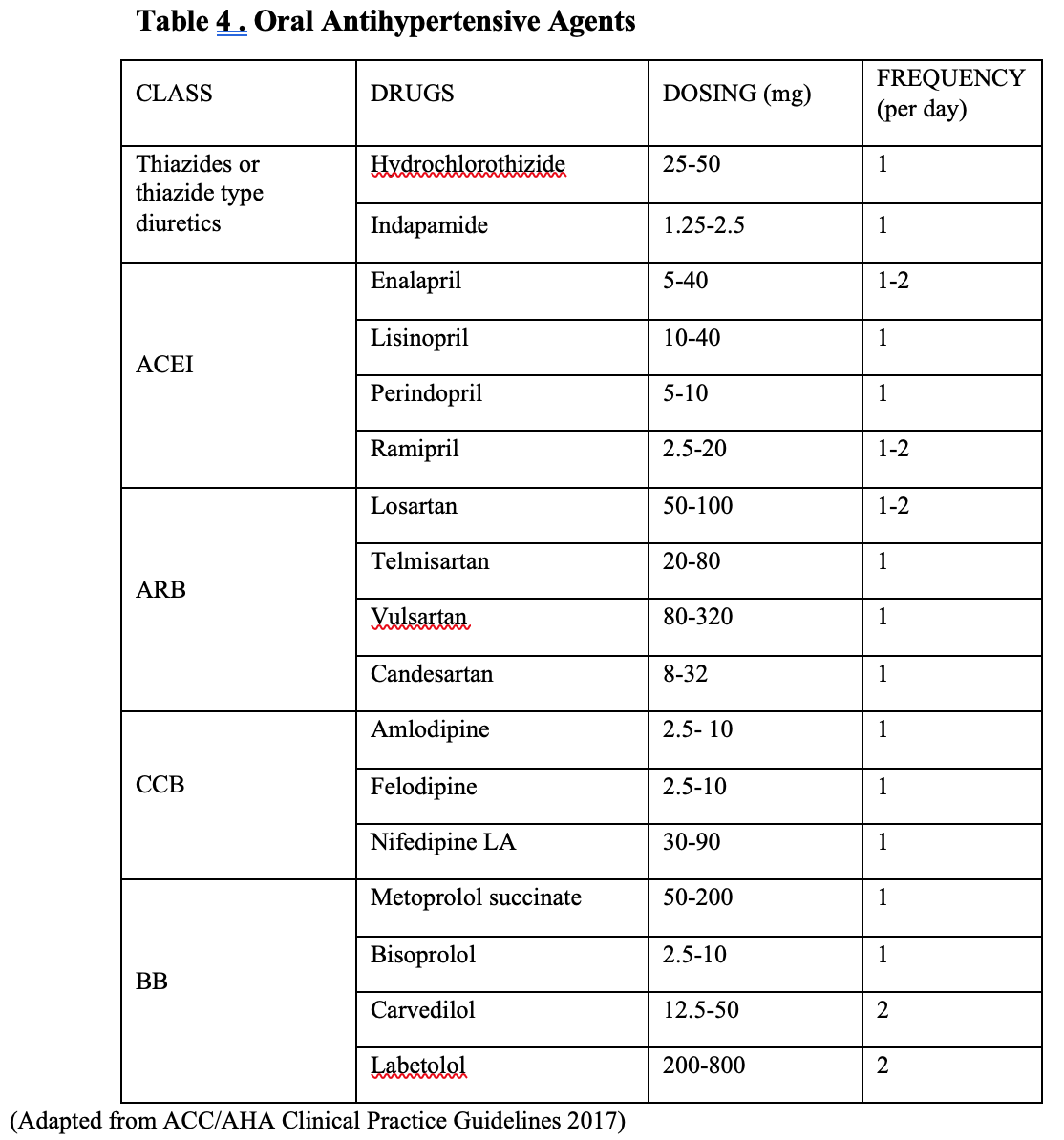
There are five major drug classes recommended for the treatment of hypertension namely thiazide diuretics, calcium channel blockers (CCB), angiotensin converting enzyme inhibitors (ACEI), angiotensin receptor blockers (ARB) and beta adrenergic receptor blockers (BB)2. (Table 4).Among which thizide diuretics, CCB, ACEI and ARB should be used as primary agents as these classes of drugs have been shown to reduce the clinical events in clinical trials. There is inadequate evidence to support the initial use of beta blockers for hypertension in the absence of specific cardiovascular co-morbidities they are reserved for conditions when there is a specific indication for their use, e.g. heart failure, angina, post-myocardial infarction, atrial fibrillation, or younger women with, or planning, pregnancy5.
CO-MORBIDITIES AND COMPELLING INDICATIONS / CONTRAINDICATIONS FOR THE CHOICE OF ANTIHYPERTENSIVE DRUGS
Certain co-morbid conditions may affect the clinical decision making of hypertension and choice of medications. The selection of medications for use in treating high BP should be guided by their use for other compelling indications and contraindications. (Table 5) Compelling indications for specific therapy involve high-risk conditions that can be direct sequelae of hypertension or commonly associated with hypertension8.

TWO-DRUGSCOMBINATION THERAPY
Traditionally, pharmacotherapy for hypertension was initiated with monotherapy. If treatment target was not achieved the dosage may be increased to maximum or drug may be changed sequentially to other classes before using combination of drugs. This step-care approach can result in therapeutic inertia with subsequent failure of treatment.
In compared to treatment regimes with initial monotherapy, initiation with two-drug combination therapy is associated with greater reduction of blood pressure with steep dose-pressure response relationship without significant increase in hypotensive episodes. It can result in more frequent blood pressure control and better adherence to treatment9.
ESC/ESH 2019 guidelines recommended initiation with two-drug combination in all patients requiring pharmacotherapy except in patients who have CVD risk with high normal BP, who are very old or frail. ACC/AHA 2017 guidelines recommended the use of combination therapy in stage 2 hypertension and average blood pressure more than 20/10 mmHg above their blood pressure targets.
INITIATION OF TREATMENT (LIFE STYLE CHANGES AND MEDICATIONS)
ESC/ESH 2018 recommended that life style advice should be given to all patients including those with high normal blood pressure. Drug treatment should be started immediately after the diagnosis of grade 2 and grade 3 hypertension. Immediate drug treatment should also be considered for patients with grade 1 hypertension associated with high or very high risk and patients with CVD, chronic kidney disease (CKD) or with hypertension mediated target organ damage (HMOD).
For those with grade1 hypertension and low or moderate risk or without CVD, CKD and HMOD, drug therapy may be delayed for 3-6 months with life style changes. Drug therapy may be considered in patients who have high normal BP and high risk or in presence of CVD especially coronary artery disease.
Core drug-treatment strategy for hypertension (ESC/ESH 2018)
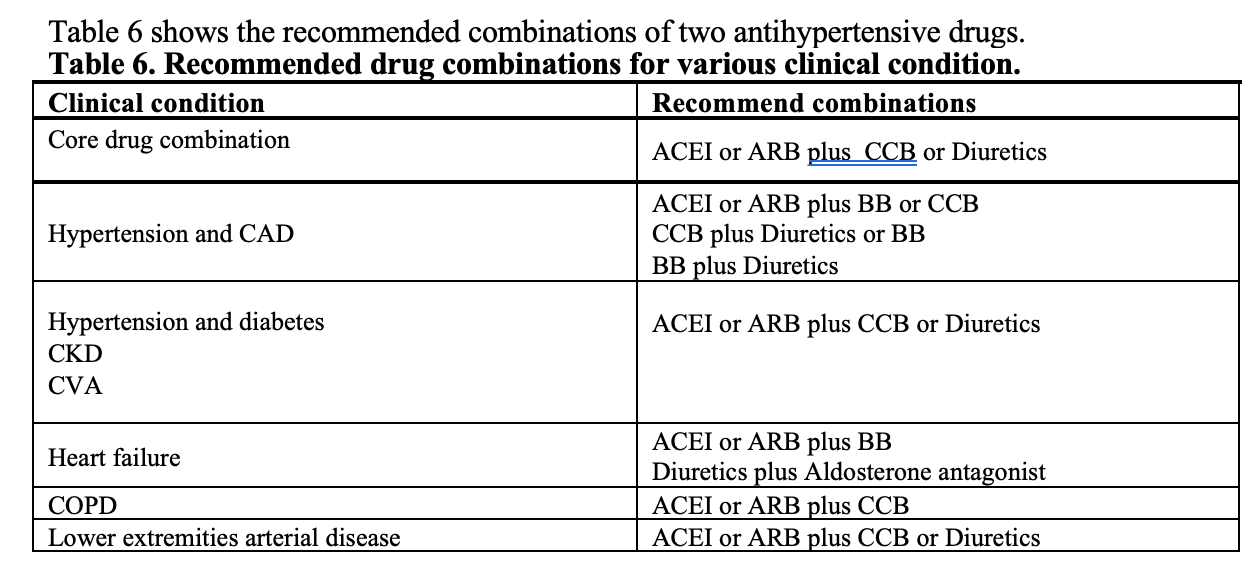
Except for the patients with grade 1 hypertension and low risk, very old or frail elderly, drug therapy should be initiated with two drug combination comprises of ACEI or ARB plus CCB or thiazide diuretics (see Table 6). When target BP is not achieved, stepped up to triple therapy comprises of ACEI or ARB plus CCB plus diuretics. If hypertension is still resistant (target not achieved) spironolactone (25-50 mg/d) or other classes like alpha adrenergic receptor blockers or beta blocker can be added as fourth agent. For better compliance, two-drugs or three-drugs combination should be given as a single pill preparation if it is available.
Use of beta-blockers can be considered at any treatment step of treatment when there is specific indication for their use, e.g. heart failure, angina, post-myocardial infarction, atrial fibrillation, or younger women with, or planning, pregnancy.
STRATEGIES TO IMPROVE THE TREATMENT ADHERENCE
Once daily dosing of medication
It is always challenging to take medicine regularly particularly with the regimen requiring multiple daily dosing. Medication adherence is greatest with once-daily dosing. In adults with hypertension, dosing of antihypertensive medication once daily rather than multiple times daily is beneficial to improve adherence5.
Single-pill combination therapy
In low and middle income countries, more than 70% of peoples who are receiving treatment for hypertension failed to achieve the target blood pressure goal. On major reason is that while majority of patients require two or more medications, most patients receive monotherapy only8. Fixed-dose combinations, also known as single-pill combinations, which incorporate two antihypertensive drugs or more into one pill, can improve control rates without increasing the risk of adverse events, and can thereby prevent millions of cardiovascular and other complications of uncontrolled blood pressure10. Current guidelines endorsed the recommendation to use single pill combination of two or three antihypertensive agents to reduce the pill burden and thereby improving the drug adherence2. Fixed dose combination antihypertensive agents proposed for inclusion in essential medicine list of WHO are ACEI and thiazide or thiazide like diuretics, ACEI and CCB, ARB and CCB and ARB and thiazide or thiazide like diuretics11.
Role of physicians
Physicians should information on the risks of hypertension and the benefits of treatment, as well as agreeing a treatment strategy to achieve and maintain BP control using lifestyle measures (information material, programmed learning, computer-aided counseling). Feedback on behavioral and clinical improvement should be provided to the patients. Individual barriers to adherence should be assessed and acknowledged. Physicians should work in collaboration with other health care providers like nurses and pharmacists2.
Health system level
Monitoring systems (telephone follow-up, home visits, tele-monitoring of home BP) should be developed. Accessibility to medication and reimbursement of single-pill-combination should be improved2.
CONCLUSION
An optimal balance between the magnitude of achieved BP reduction and the tolerability of treatment in the single patient should be pursued in daily clinical practice rather than fixing rigid BP target or safety boundaries. Eventual management of each individual needs to be carefully tailored to their needs and depends upon the relationship that exists between the physician and patient.
BIBILOGRAPHY
- Kjeldsen SE (2017) Hypertension and cardiovascular risk: General aspects. Pharmacol Res. 2018 Mar;129:95-99. doi: 10.1016/j.phrs.2017.11.003. Epub 2017 Nov 7
- European Society of Cardiology Task Force (2018) ESC/ESH Guidelines for the management of arterial hypertension. Eu Heart J (2018) 39, 3021–3104
- Robert M. Carey, Paul K. Whelton (2018) Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Synopsis of the 2017 American College of Cardiology/American Heart Association Hypertension Guideline. Ann Intern Med. 2018;168(5):351-358. DOI: 10.7326/M17-3203
- American College of Cardiology/American Heart Association Task Force on Practice Guidelines (2013) ACC/AHA Guideline on the Assessment of Cardiovascular Risk. Circulation 2013 Volume 129, Issue 25_suppl_2
- European Society of Cardiology (2003) Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project Eu Heart J 2003;24:987-1003
- WHO. WHO/ISH Risk Prediction Chart 2007
- Appel LJ (2003) J Am Soc Nephrol 14: S99–S102, 2003
- US Department of Health and Human Services (2004) The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. August 2004
- WHO(2019) Fixed-dose combination antihypertensives. 2nd Expert Committee on the Selection and Use of Essential Medicines 2019
- Kishore SP, Salam A, Rodgers A, Jaffe MG, Frieden T(2018) Fixed dose combination for hypertension (correspondence) Lancet September 8, 2018 p. 819-820
- Mancia G, Rea F, Corrao G, Grassi G (2019) Two-drug combinations as first-step antihypertensive treatment. Circ Res. 2019;124:1113-1123.
Myo Lwin Nyein
MBBS, M Med Sc (Int. Med.) FRCPE, DTM&H
Former Professor of Medicine
University of Medicine 2 Yangon
Vice President
Myanmar Society of Hypertension



