Thyroid function tests are used in a variety of clinical settings:
- to evaluate thyroid dysfunction
- assess the adequacy of thyroid hormone therapy and
- monitor the treatment of hyperthyroidism
Assuming steady-state conditions and the absence of pituitary or hypothalamic disease, thyroid function is best assessed by measuring serum TSH.
However, measurement of serum TSH and thyroid hormone levels remains important in patients with symptoms of possible thyroid dysfunction since a normal serum TSH does not unequivocally exclude the possibility of central hypothyroidism or central hyperthyroidism from a TSH secreting tumor.
Thyroid function is assessed by one or more of the following tests:
- Serum TSH concentration
- Serum total T4 and T3 concentrations
- Serum free T4 and T3 concentrations
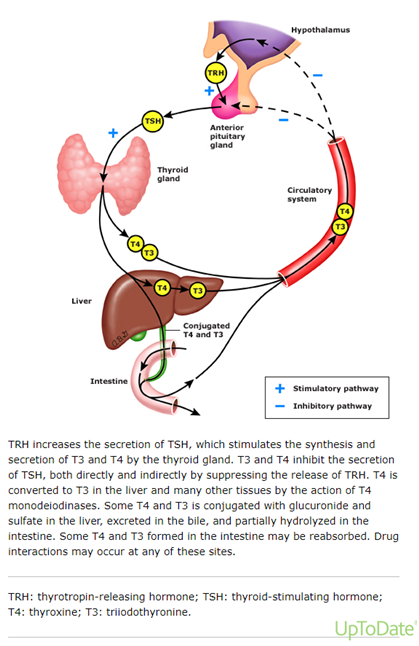
Regulation of thyroid hormone production
Reference range – There is considerable controversy as to the appropriate upper limit of normal for serum TSH. Most laboratories have used values of approximately 4.5 to 5.0 mU/L. The distribution of TSH values in the population differs by age. Lower TSH target is also used during pregnancy.
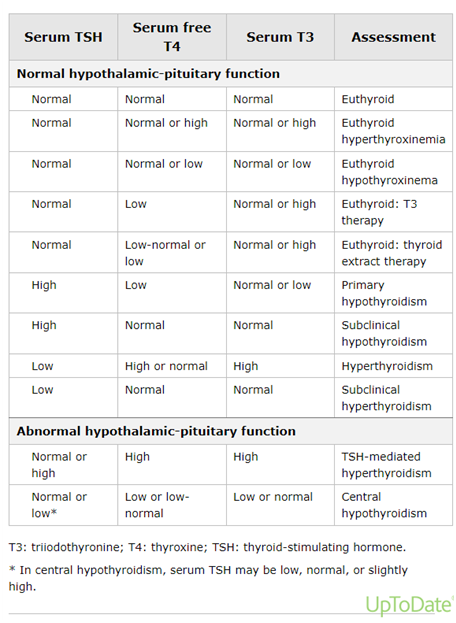
Patterns of thyroid function tests during assessment of thyroid function
Assay interference with biotin ingestion — Patients taking biotin should hold the supplement for two days prior to assessing thyroid function and longer if they are taking more than 10 mg a day.
Some automated assays for measurement of thyroid tests utilize a biotin-streptavidin separation system. Patients who are ingesting 5 to 10 mg of biotin (eg, marketed over the counter to prevent hair loss) can have spurious results in these assays. Biotin may cause falsely low values in immunometric assays (eg, used to measure TSH), and falsely high values in competitive binding assays (eg, used to measure free T4, T3, and free T3, and TSH receptor-binding inhibitor immunoglobulin [TBII or TBI])
Outpatient setting
To assess possible thyroid dysfunction in an individual patient:
Measure both serum TSH and free T4 if pituitary or hypothalamic disease is suspected (eg, a young woman with amenorrhea and fatigue).
Measure serum free T4 if the patient has symptoms of hyper- or hypothyroidism despite a normal TSH result.
Serum TSH assays are both more sensitive and specific than serum free T4 measurements for outpatients if a single test is utilized. However, some experts recommend that both serum TSH and free T4 be measured in all patients for evaluation purposes since errors may be made when only TSH is measured in patients with secondary or central hypothyroidism or TSH-mediated hyperthyroidism.
Inpatient setting
Evaluating thyroid function in the inpatient setting is a more difficult problem, and it is not recommended unless thyroid disease is strongly suspected, since changes in thyroid hormones, binding proteins, and TSH concentrations occur in severe nonthyroidal illness.
These changes may include:
- Low concentrations of all three binding proteins
- High concentrations of free fatty acids that displace thyroid hormones from binding proteins
- Acquired central hypothyroidism
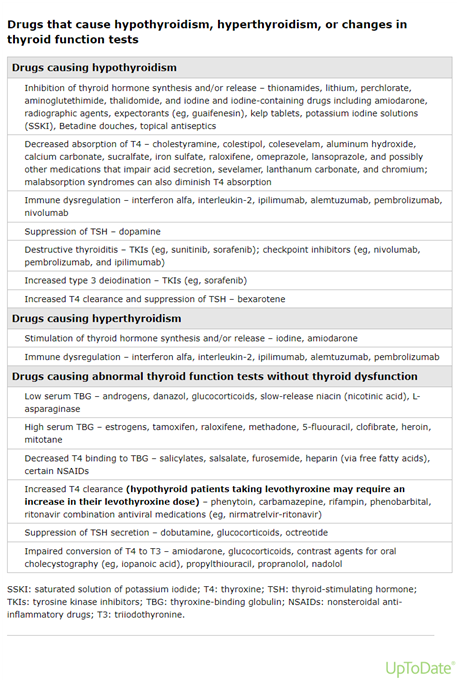
- The patient may be receiving medications that affect thyroid function
While there are advocates for either serum TSH or free T4 being more useful in inpatients, most experts suggest that both serum TSH and free T4 or total T4 are necessary to assess thyroid function in hospitalized patients.
Monitoring levothyroxine therapy
One of the more common reasons for assessing thyroid function is to assess the adequacy of levothyroxine therapy.
- Primary hypothyroidism – Patients with primary hypothyroidism who are taking levothyroxine replacement therapy can be monitored by assessing the serum TSH only. In general, serum free T4 measurements are very insensitive for assessing the appropriateness of the levothyroxine dose. Doses of levothyroxine that are 40 percent higher than optimal may result in subnormal serum TSH concentrations, yet serum free T4 concentrations frequently remain within the normal range. Nevertheless, free T4 measurements can be useful to determine appropriate dose increases or decreases when TSH is very high or low, respectively.
- Liothyronine (T3, Cytomel) is generally not recommended for treating hypothyroidism. However, in patients with persistent hypothyroid symptoms on levothyroxine monotherapy, T3 is sometimes added. In this setting, we do not routinely monitor T3 levels. With the currently available T3-containing preparations, there are wide fluctuations in T3 concentrations throughout the day due to its rapid gastrointestinal absorption and its relatively short half-life in the circulation (approximately one day).
- Secondary hypothyroidism – The one setting in which the serum free T4 value should be used to titrate the thyroid hormone dose is in patients with secondary hypothyroidism due to pituitary or hypothalamic disease who have absent or impaired TSH release. In this situation, the free T4 level should be maintained in the upper 50 percent of the normal range.
- Thyroid cancer – The goal and requirement for monitoring are different in patients taking levothyroxine for suppression of TSH secretion to prevent recurrence of thyroid cancer.
- Thyroid nodules and goiter – Rarely, mild suppression of TSH with levothyroxine is used to prevent growth or regrowth of goitrous tissue.
Monitoring treatment of hyperthyroidism
During the early treatment of hyperthyroidism with antithyroid drugs, radioiodine, or surgery, serum TSH may remain subnormal for several weeks and rarely for several months. Initial monitoring of therapy, therefore, should consist of periodic clinical assessment, measurements of serum free T4, and often measurements of total T3 levels.
Serum T3 concentrations may be disproportionately higher than serum T4 concentrations in many types of hyperthyroidism. Also, serum free T4 levels may normalize with antithyroid drug therapy, while serum T3 levels may remain persistently elevated. Once steady-state conditions are assured, measurement of serum TSH only can be used to assess the efficacy of therapy.
Antithyroid antibodies
Several antibodies against thyroid antigens have been described in chronic autoimmune thyroiditis and Graves’ disease. However, routine measurement of antithyroid antibodies is not necessary for the assessment of thyroid function.
- Thyroglobulin (Tg, formerly known as the colloid antigen) – Tg is synthesized by follicular cells and secreted into the lumen of the thyroid follicle, where it is stored as colloid. Patients with Hashimoto’s thyroiditis or Graves’ disease may have thyroglobulin antibodies, but thyroglobulin antibodies do not need to be measured to diagnose autoimmune thyroid disease. However, thyroglobulin antibodies can interfere with the measurement of serum thyroglobulin, and they are therefore always assessed when monitoring serum thyroglobulin levels in patients with differentiated thyroid cancer. (Thyroglobulin is used for the detection of residual, recurrent, or metastatic disease.)
- Thyroid peroxidase (TPO, formerly known as the microsomal antigen) – TPO catalyzes the iodination of tyrosine residues of Tg to form monoiodotyrosine and diiodotyrosine. Nearly all patients with Hashimoto’s thyroiditis have high serum concentrations of TPO antibodies. Serum anti-TPO antibodies need not be measured in patients with overt primary hypothyroidism, because almost all have chronic autoimmune thyroiditis. However, a test for anti-TPO antibodies may be useful to predict the likelihood of progression to permanent overt hypothyroidism in patients with subclinical hypothyroidism.
- The TSH receptor – Thyrotropin receptor antibodies (TRAbs) are classified as stimulating, blocking, or neutral. Stimulating antibodies (thyroid-stimulating immunoglobulins, TSI) cause Graves’ disease. Thyroid receptor-blocking antibodies can cause hypothyroidism. Some patients will have a mixture of both antibodies, and, depending on the relative titers of these antibodies, they may fluctuate between hyperthyroidism and hypothyroidism. Neutral antibodies bind the receptor but do not stimulate or block function.
There are two methods for measuring TRAb:
- TSI assays measure only thyroid-stimulating antibodies
- TSH receptor-binding inhibitor immunoglobulin (TBII or TBI) assays measure stimulating, blocking, and neutral antibodies.
Third-generation TSI assays have a sensitivity of 97 percent and a specificity of 99 percent for the diagnosis of Graves’ disease. Some third-generation TBII assays are automated and less expensive but are not specific for stimulating antibodies.
Measurement of TRAb is unnecessary for establishing the cause of hyperthyroidism if a radioiodine uptake has been obtained. However, TRAb measurements are being used increasingly as an alternative to obtaining a radioiodine uptake when Graves’ disease is suspected. TRAb measurements are also useful for assessing the likelihood of remission after a 12- to 18-month course of antithyroid drugs in patients with Graves’ disease, and many experts will obtain a baseline measurement early in the course of antithyroid drug treatment.
When considering the presence of blocking antibodies in patients with fluctuating hyper- and hypothyroidism (or initial hyperthyroidism, followed by hypothyroidism), a negative TSI level and a positive TBII level, or a TBII level that is considerably higher than the TSI level, is indirect evidence for the possible presence of blocking antibodies.
Reference
UpToDate Topic 7891 Version 40.0 (Sept 2023)
Author Information
Nandar Min Swe
Attending Physician/Consultant Endocrinologist
LA, USA