Managing Diabetes Mellitus For Safe Home Stay In COVID-19 Era
Introduction
Since WHO declared the novel COVID-19 outbreak as a global pandemic on 11 March 2020, there are no countries in the world to be exempted from COVID- 19 infections and the highest prevalence and biggest mortality are seen in USA, Brazil , India and Russia . Although the vaccines production reached to stage 3 in some developed countries, the earliest time to be available around the world would be mid 2021. There is no doubt that developing countries would face the problem of universal coverage. Hence WHO still recommends the possibility of second wave infections and suggest to continue highly vigilant infection control measures like wearing masks, social distancing, hand hygiene and washing, and avoiding crowded places.
Among the deceased persons with COVID- 19, patients with diabetes and non-communicable diseases are the majority. Studies from UK and USA have shown that diabetes is one of the common risk factors for severe COVID-19 infection and its death. Presences of diabetes itself do not increase the prevalence of COVID -19 infection, but poor glycemic control with comorbidity is a risk factor for severity and mortality.
Why COVID -19 infection make hyperglycemia getting worse can be explained by the influence of stress hormones and also due to adverse effect of medications used during the illness. COVID-19 infection in people with or without previously recognized diabetes increases the risk of the emergency states of hyperglycemia with Diabetic Ketoacidosis (DKA), Hyperosmolar Hyperglycemic State (HHS) and mixed type. Once infected with virus, hyperglycemia can lead to increased complications, respiratory distress, vascular thrombosis, cardiac toxicity, multi-organ failure and high mortality in hospitalized patients with COVID-19.
Until now, Myanmar has been lucky enough not to face mass fatalities compared to border Countries and having only 6 deaths out of 395 positive cases until first week of August. There is an emergence of second wave of COVID infections found in Korea, Japan, Australia and increasing deaths are seen in India and Bangladesh which are neighbor countries of Myanmar. Hence, there is still recommendation for precautionary measures to stay safe with new normal life style in this period.
Sadly since mid August, local transmission outbreak started in Sittwe, the capital of Rakhine state, and there is a growing prevalence of positive cases across Western part of Myanmar because of virus mutation to rapidly infective G 614 strain. Therefore, every parts of Myanmar have to be prepared for mass outbreak to reduce mortality in second wave infections.
In align with various endocrine associations across the world, Myanmar society of Endocrine and metabolism (MSEM) and Myanmar Medical Diabetic Association (MMDA) have developed “Diabetes management guideline in COVID- 19 pandemic” which mainly focus on PUI cases and hospitalized patients. As Myanmar is facing increasing burden of non-communicable disease, this is a high time for alert and raising awareness of people with Diabetes to prevent unnecessary complications and fatalities during second wave COVID-19 infections. Severe illness and mortality is more vulnerable to older people and those with multiple comorbidities such as diabetes, hypertension and cardiovascular disease. Hence this standard operating procedure would be beneficial for family physicians and basic health care providers to follow in the care of people with diabetes in new normal period.
What cautions to be made for people with Diabetes to prevent infection
- People with diabetes in the community who have not yet been infected with the SARS-CoV-2 virus should intensify their metabolic control as much as possible
- Monitor SMBG at least twice per day and more to be made when the person is ill and having fever: Target levels: pre-meal glucose (100-140 mg %), post prandial glucose
(not more than 180 mg %) - Take plenty of oral fluids to maintain good hydration
- Keep regular nutritious diet, but if appetite reduced with fever, take food ‘little and often’, don’t skip the meals
- Have daily foot checks to ensure early detection of poor blood supply, infection and regular changes of dressings for foot ulcers
- Check body temperature if they feel like they have a fever, sore throat and have an emergency contact number to family physicians for first aid measures
- Continue usual diabetes and hypertensive medication and keep enough 1 month supply
- If necessary, primary care doctors or specialist physicians could help patients to adjust anti-diabetic medications by phone or via online-consultation.
- Ensure to take strict infection control measures: wearing masks, hand washing etc
Type 1 DM patients
Continue usual basal insulin dose and adjust the bolus insulin according to oral intake. If frequent injections are not possible in the absence of care person, better to switch to twice daily pre mix injection pens.
Type 2 DM patients
Among the usual oral hypoglycemic agents, judiciously use the most physiological oral hypoglycemic agent with least side effects during the infection.
Sulphonylurea and insulin secretagogues are to be used with caution because of risk of hypoglycemia in the illness time.
SGLT 2 inhibitors can lead to diabetes ketoacidosis in the state of fever and dehydration so is best avoided.
Metformin can be used with caution and should be avoided in renal impairment and metabolic decompensation to avoid lactic acidosis.
DPP4 inhibitor is the only agent which can be safely used as less chance of hypoglycemia and renal side-effects. GLP1 agonists must be used in caution with GI symptoms.
Anti-hypertensives can be continued including ACEI, ARB, diuretic unless renal function declines.
Sick day rules
- If they develop Coronavirus symptoms or any other illness, it is likely to affect their blood sugars into either hypo or hyperglycemia
- While unwell, it is very likely they will need more insulin in those with type1 DM, so even if they are vomiting, don’t stop insulin, seek help from family doctors
- Monitor blood sugar level and blood or urine ketone every 4-6 hours
- Drink at least 100 ml of water or sugar-free liquids every hour
- Do not fast. Try to eat some food which contains carbohydrate e.g. milk, toast, cereal
- Check glucose four hourly and adjust the insulin dose or oral hypoglycemic agents
- If vomiting continues and blood ketones found to be positive >1.5mmol/L or urine ketone
≥+2, send the patients to emergency.
Treatment of hypoglycemia
If blood glucose is less than 70 mg/dl, if patient is not unconscious,
* Treat with 15-20g fast acting carbohydrate for immediate measures. Examples include: Half a can of sugary drink , Fruit juice 200mls , 5 spoonful sugar in warm water , one chocolate bar
* After treating the hypoglycemia, ask to eat 15-20g of slower acting carbohydrate. Sandwich, bowl of cereal, a glass of milk 200mls, an apple or orange.
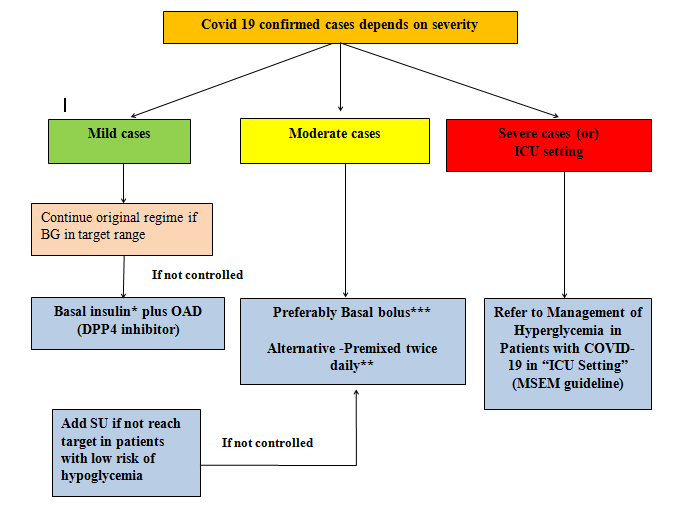
What treatment should be used once infected with COVID-19 infections
In suspected case – previous medication regime must be evaluated and followed as appropriate, take antioxidants and good nutrition to boost the immune response, no need for hospitalization unless in emergency, self-isolation and home quarantine is enough.
Ordinary COVID-19 positive case – once swab is positive and put under surveillance in facility quarantine area, subcutaneous once daily basal insulin or premix insulin twice daily injections are preferred with self-monitoring blood glucose 6 hourly if not controlled well with usual oral regime.
Severe or critically ill COVID-19 case- IV insulin infusion therapy may be preferred treatment to combat severe hyperglycemia and cytokine storms. (Refer to MSEM guideline of management of DM with COVID-19 2020)
Figure 1. Glycemic Management of COVID 19 confirmed case according to severity of infection
References:
ADA, American Diabetes Association (2020) The Standards of Medical Care in Diabetes-2020.Diabetes Care, 43, Supplement 1, pp. S1-212.
Association, A.D. (2019) . Diabetes Care in the Hospital: Standards of Medical Care inDiabetes—2019. Diabetes Care. 42 (Supplement 1), S173–S181.
A Covid-19 Response Action – Diabetes Management in Care Homes[Internet].A NationalStakeholders Covid-19 Response Group Interim Guidance. 2020[cited 3-5-2020]. Available from: https://abcd.care/sites/abcd.care/files/site_uploads/Resources/COVID- 19/Covid-19-and-Diabetes-Care-Home-Guidance-28042020.pdf.
Banerjee, M.,Chakraborty, S. & Pal, R., (2020) Diabetes self-management amid COVID-19pandemic. Diabetes MetabSyndr, 14, pp.351-354.
Covid-19 report of MOHS, Ministry of Health and Sport, Myanmar 2020. Available:https://www.mohs.gov.mm.
Consensus Guideline for the Management of Diabetes during COVID-19 Pandemic (2020) Guideline Developing Committee and Advisory Group for the Management of Diabetes duringCOVID – 19 Pandemic, Myanmar.