Introduction
Malaria remains a major global health concern, particularly in endemic regions, where artemisinin-based combination therapy (ACT) is the standard treatment for uncomplicated cases. While ACT is highly effective in clearing the malaria parasite, some patients experience post-treatment fever, raising concerns about treatment failure or recurrence. However, not all post-treatment fevers are due to malaria, and misattributing them to persistent infection can lead to unnecessary retreatment and mismanagement.
Case report
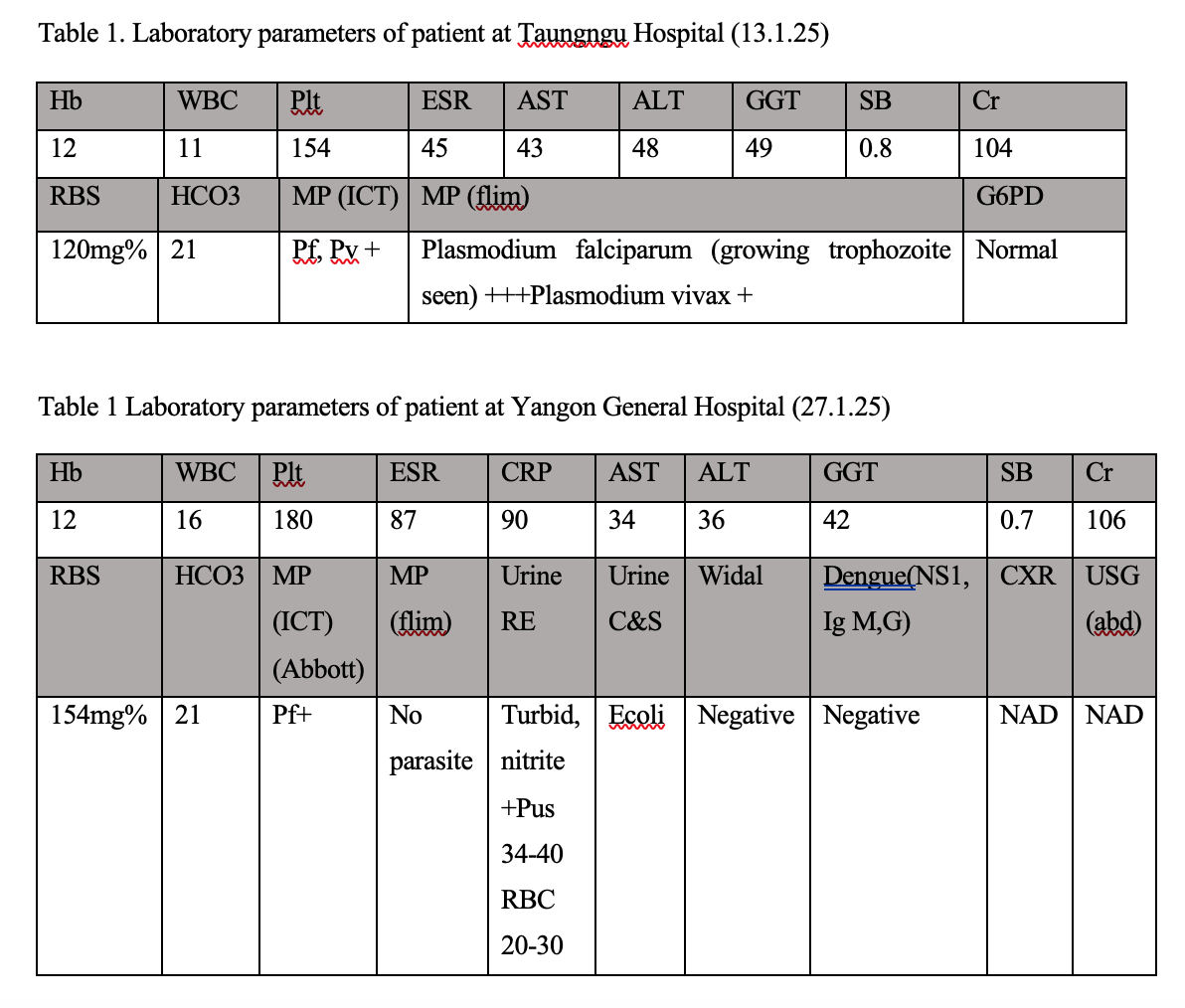
A 49-year-old man, a woodworker, from Taungnguu District, Bago division was admitted to Tropical and Infectious Disease Department, Yangon General Hospital on 27th January 2025 with a chief complaint of fever x 2 days, headache and fatigue for 1 day duration. Fever was high grade and associated with chills but no rigor. No positive symptoms in respiratory, cardiovascular, gastrointestinal, rheumatology systems except for incomplete senses of urination. Headache occurred at times of high fever but no other CNS symptoms like limb weakness, fits or blurred vision were reported. Regarding past medical problems, he was recently discharged (2 weeks ago) from a private hospital at Taungnguu district for high fever with chills and rigor for 5 days while he was working in the Bago Range. Except for headache, no fits or loss of consciousness were present at that time. He was diagnosed as uncomplicated malaria due to plasmodium falciparum and plasmodium vivax positive in RDT and film report. Laboratory investigation at that time is attached. (table 1) He was treated with ACT (Coartem, artemether and lumefantrine) 4 tablets twice a day for 3 days followed by PO primaquine 0.25mg/kg for 14 days. After treatment, the fever subsided and he was discharged. Two weeks after discharge, he had fever and headache again and came to Yangon for fear of cerebral malaria. On examination, clinically stable except for temperature of 100’F. Laboratory investigations were done to find out the cause of fever. (Table 2) To rule out recurrence of malaria infection, RDT and thick and thin blood films examination were done. On RDT test, plasmodium falciparum was still positive but not plasmodium vivax and there were no malaria parasites on peripheral blood film examination. He was treated with IV ceftriaxone 1g 12 hrly for possible urinary tract infection because of nitrite positive and 34-40 pus cell in urinalysis. Fever subsided after 48 hr of treatment and urine C&S revealed Ecoli infection. He was discharged after 4 days and follow up was planned at Infection Clinic at YGH.
Discussion
Persistent Plasmodium falciparum (Pf) positivity on a rapid diagnostic test (RDT) after malaria treatment can occur due to several reasons, even when the infection has been successfully cleared. The key causes include: 1,2
1. Persistent HRP2 Antigen (Histidine-Rich Protein 2) Detection• Most Pf RDTs detect the HRP2 antigen, which can remain in the bloodstream for weeks to months after successful treatment, even in the absence of active infection• The antigen clearance rate varies among individuals but can persist for up to 5–6 weeks, leading to false-positive results.
2. True Treatment Failure 3Recurrence of P. falciparum malaria can be the result of a re-infection, or a recrudescence (i.e failure). If fever and parasitaemia fail to resolve or recur within 28 days of treatment then this is considered a failure of treatment. Treatment failure must be confirmed parasitologically – preferably by blood film examination. Recurrence of fever and parasitaemia more than two weeks after treatment due to recrudescence or new infection. It can only be made through parasite genotyping by PCR. Since PCR is not routinely used in patient management, to simplify drug deployment, all presumed treatment failures after two weeks of initial treatment should be considered as new infections, especially in areas of high transmission.
3. RDT Cross-Reactivity• Some RDTs may cross-react with other conditions (e.g., rheumatoid factors, other infections) leading to false-positive results• Cross-reaction with other Plasmodium species (e.g., P. malariae) co-infections can also occur.
4. Delayed Parasite Clearance• Some patients may take longer to completely clear all malaria parasites from their blood, leading to low-level parasitemia detectable by RDTs but not necessarily causing illness. Confirming True Infection vs. False Positivity, a microscopy blood smear or PCR test should be done to confirm active infection if RDT remains positive.
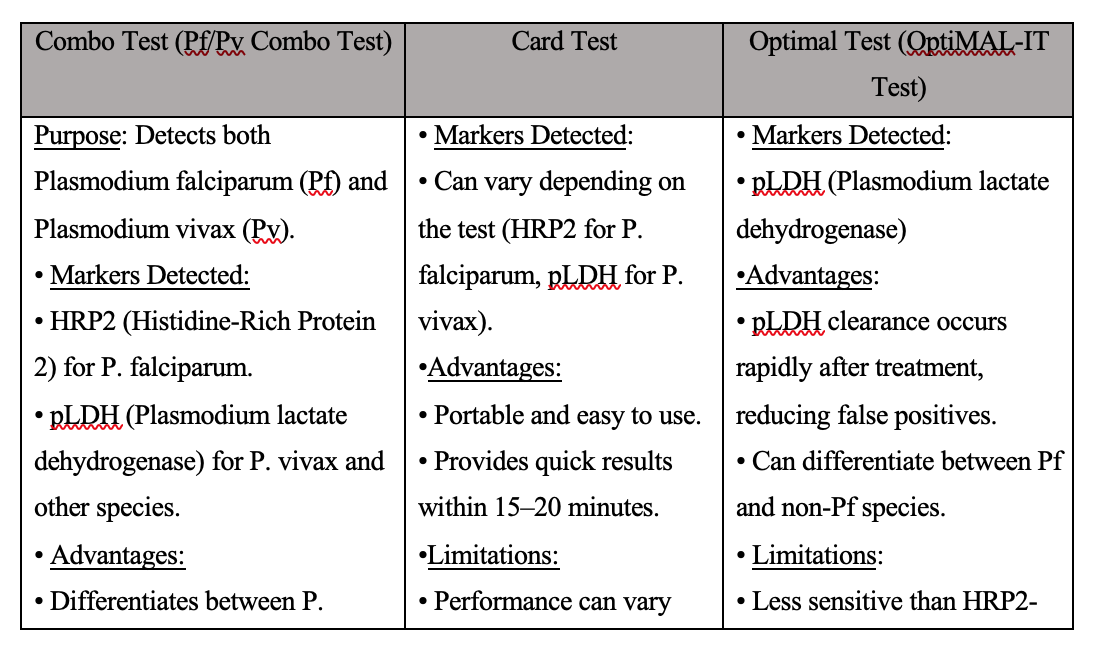
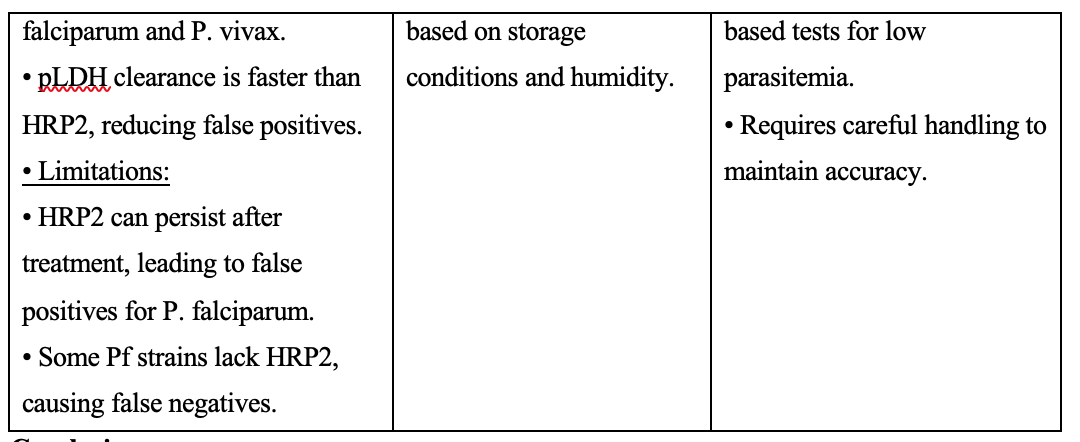
Comparison of available RDT in Myanmar 4,5,6
Conclusion
While malaria is a common cause of fever in endemic regions, persistent or recurrent fever after complete ACT treatment should prompt clinicians to explore other potential diagnoses. This case emphasizes the importance of thorough clinical assessment, as attributing post-treatment fever solely to malaria could lead to missed diagnoses and inappropriate management. A systematic approach, including laboratory investigations and consideration of alternative infectious and non-infectious causes, is crucial for ensuring accurate diagnosis and optimal patient care.
References
1. Oulton, T., Mahamar, A., Sanogo, K. et al. Persistence of Plasmodium falciparum HRP-2 antigenaemia after artemisinin combination therapy is not associated with gametocytes. Malar J 21, 372 (2022). https://doi.org/10.1186/s12936-022-04387-0
2. Lee JH, Jang JW, Cho CH, Kim JY, Han ET, Yun SG, Lim CS. False-positive results for rapid diagnostic tests for malaria in patients with rheumatoid factor. J Clin Microbiol. 2014 Oct;52(10):3784-7. doi: 10.1128/JCM.01797-14. Epub 2014 Jul 23. PMID: 25056333; PMCID: PMC4187788.
3. GUIDELINES FOR MALARIA DIAGNOSIS AND TREATMENT IN MYANMAR, 2015
4. Eticha T, Tamire T, Bati T. Performance Evaluation of Malaria Pf/Pv Combo Test Kit at Highly Malaria-Endemic Area, Southern Ethiopia: A Cross-Sectional Study. J Trop Med. 2020 Sep 7;2020:1807608. doi: 10.1155/2020/1807608. PMID: 32963553; PMCID: PMC7492921.
5. P Gendrot, M.; Madamet, M.; Fonta, I.; Benoit, N.; Amalvict, R.; Mosnier, J.; French National Reference Centre for Imported Malaria Study Group; Pradines, B. Comparative Assessment of the Sensitivity of Ten Commercial Rapid Diagnostic Test Kits for the Detection of Plasmodium. Diagnostics 2022, 12, 2240. https://doi.org/10.3390/diagnostics12092240
6. Palmer CJ, Lindo JF, Klaskala WI, Quesada JA, Kaminsky R, Baum MK, Ager AL. Evaluation of the OptiMAL test for rapid diagnosis of Plasmodium vivax and Plasmodium falciparum malaria. J Clin Microbiol. 1998 Jan;36(1):203-6. doi: 10.1128/JCM.36.1.203-206.1998. PMID: 9431947; PMCID: PMC124834.
Author Information
Aye Mya Theingi Win1, Khin Rupar Ko2, Aye Aye Win3 , May Zabe1, Nyunt Thein4
1. Senior Consultant physician, Tropical and Infectious Diseases Department, Yangon General Hospital
2. Professor, Tropical and Infectious Diseases Department, Yangon General Hospital
3. Associated Professor, Tropical and Infectious Diseases Department, University of Medicine (1), Yangon
4.Senior Consultant physician, Former Head of Department of Medicine, Emeritus Professor of Medicine, University of Medicine (1), Yangon