Use of I.U.D in Myanmar

(First published in MJCMP (1), pp 47- 52, 1996)
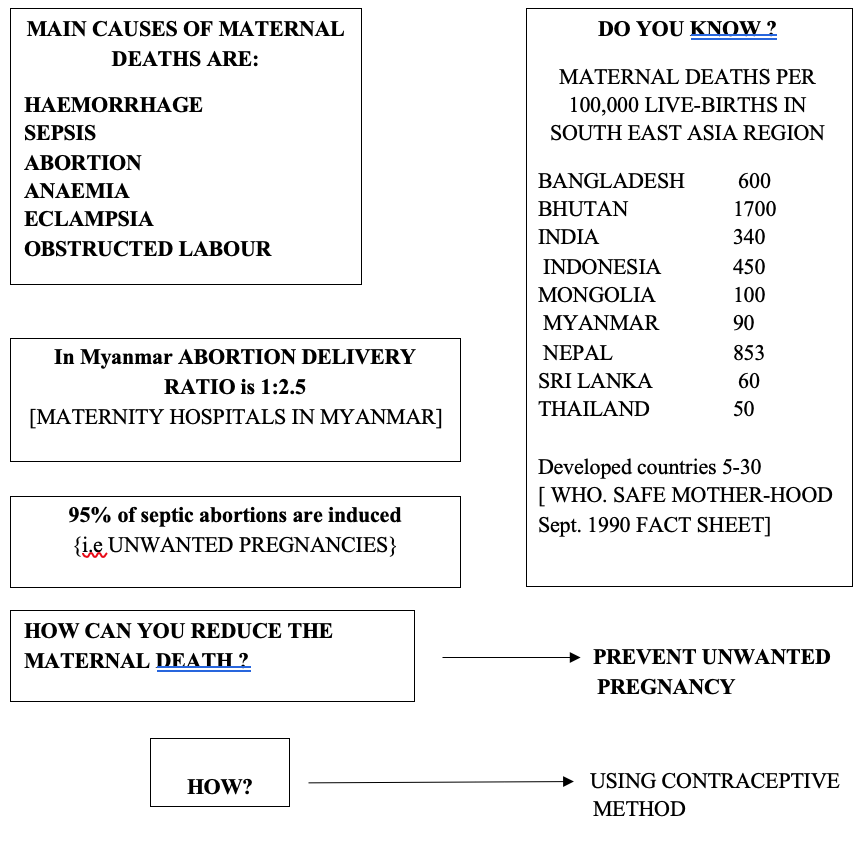
Today, the rate of maternal mortality in rich and poor countries shows greater disparity than any other public health indicator.
For successful family planning we need counselling. Counsellors who usually are doctors or nurses should explain to the users, the available methods, their risks, advantage and disadvantages of contraceptives.
In Myanmar, some of the young girls and elderly women are taking contraceptive pill without consulting any medical personnel. This results in severe complications, such as breast carcinoma, hypertension and ischemic heart disease.
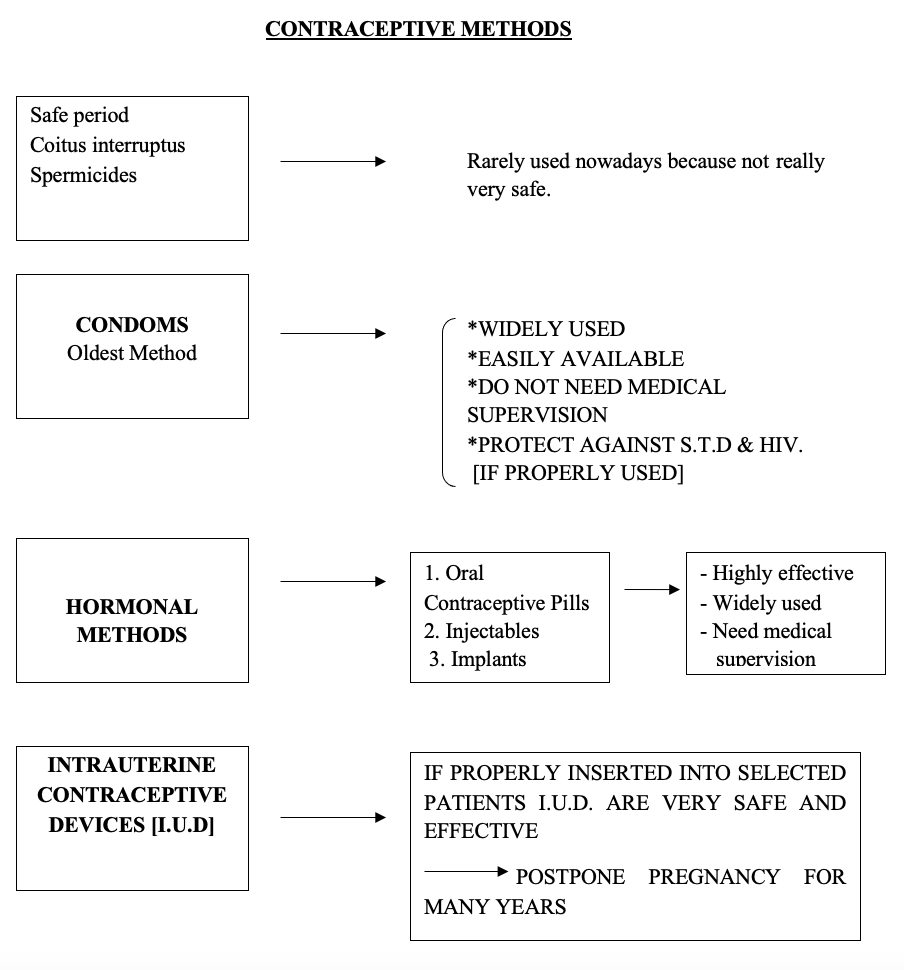
In this issue I would like to give some aspects of intrauterine contraceptive devices. The first I.U.D. designed for human contraception was developed in 1909 by a German physician Richard Richer. It was ring shaped and made of silkworm gut. The first I.U.D. to be widely used was Grafenberg’s ring made of silver wire and silkworm gut (1920). Later it was modified by different persons from OTA ring, Margulies coil, Beinberg Bow to LIPPES and TATUM.
Essentially there are three types;
Fig. I.
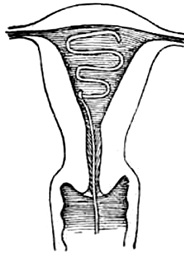
Fig. I. Inert devices such as Lippes Loop
Fig.2.
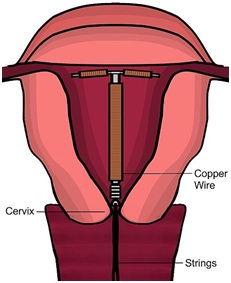
Fig.2. Devices with various applications of copper design to increase effectiveness and reduce surface area. (Copper T, Copper 7 Multiload)
Fig.3
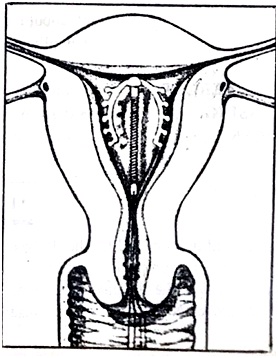
Fig.3. Medicated I.U.D.releasing low concentration of progestins and Norgestral.
One should consider the contraindications before advising someone to use IUD.

I.U.D should not be used in:
- known or suspected pregnancy
- Multiple fibroids especially if they are submucus.
- Congenital uterine abnormality.
- Acute or subacute pelvic inflammatory disease or active vaginintis.
- Gynaecological malignancy.
- Abnormal uterine bleeding.
- Valvular heart disease (Risk of bacterial endocarditis)
PROBABLY MULTIFACTORIAL
- Interference with endometrial implantation of blastocyst.
- Copper devices interfere with endometrial enzyme.[Carbonic Enhydrase]
- Probably reduce the rate of sperm ascent to the fallopian tubes.
COPPER DEVICES Lower surface area—————less uterine bleeding, tolerated by nullipara but better to avoid I.U.D in nullipara because infection can later result in infertility.
LIPPES LOOP Three different sizes———–use size “A” for small uterus.
No need to be replaced.
It should be used if one cannot be certain of patient compliance for follow up.
PROGESTERONE Require once a year replacement. Need follow up.
RELEASING Relatively unsuitable to use in Myanmar because it need
DEVICES regular supervision, it also causes break through bleeding.
Potential users of I.U.D. should be counselled before insertion. According to Grefenberg (1993) the most appropriate time for I.U.D. insertion is immediately after the menstruation. This assures that the woman is not pregnant and cervical os is still dilated providingeasy insertion and bleeding produced by insertion is masked by menstrual bleeding. In the last decade many investigators have found that it can be successfully inserted after delivery both in early and later post partum period and immediately after abortion. But expulsion rate and chances of infections are higher.
Proper insertion of 1.U.D. is critical to the success of the device. The objective of insertion is to place the device as high as possible in the endometrial cavity without perforating the myometrium. If it lies in the lower uterine cavity, uterine contraction can expel it easily. Moreover the fertilised ovum usually implants in the upper part of the uterus and unless the devices cover that area, it will not provide effective protection.

Since expulsion occur most frequently around the time of the first menstruation after the insertion, the patient should be either trained to assure the presence of the thread of the device of she should be rechecked to determine whether device is still in situ soon after her first post insertion period. Besides this and the absence of complicating symptoms, she should be rechecked once or twice a year. But as for copper bearing devices, she must be advised the need for removal and reinsertion.
PAIN & DYSMENORRHOEA – Dysmenorrhoea and increased menstrual bloods loss occur in the first two to three cycles.
IRREGULAR BLEEDING – Spotting and mid cycle bleeding may occur with progestrone releasing I.U.D. The users should be reassured about it.
But if bleeding and discomfort continue the I.U.D should be removed and alternative method should be advised.
PERFORATION – This usually occurs at the time of insertion most often through fundus or posterior surface. In large series of insertions the perforation rate is about 1: 1000.
Perforation should be suspected if the patient states that she cannot feel the tail at follow up clinic. But this may mean that the device has rotated in the uterine cavity or has been translocated.
Pelvic Ultra Sound will help locate the device.
EMBEDDING – Embedding of the I.U.D in the endometrium is sometimes encountered after prolonged use. It is usually found out of the time of removal.
INFECTION – The risk of pelvic inflammatory disease associated with I.U.D may have been exaggerated but is real. The insertion I.U.D can never be a sterile procedure and transient colonisation of endometrium is a norm for a few days after insertion.
Large study from W.H.O only shows an incidence of pelvic inflammatory disease in the first 20 days after insertion. Thereafter there is little difference between the rates in I.U.D. user and general population.
ECTOPIC PREGNANCY – Ectopic Pregnancy may be due to infection rather than the I.U.D. In a large study from Population Council it is clear that both intrauterine and tubal pregnancies are reduced by I.U.D. There is no reduction in ovarian pregnancy.(Mishell 1979).
SPONTANEOUS ABORTION Pregnancy occurring with I.U.D in situ is associated with spontaneous abortion rate of 55%. By definition, any pregnancy with I.U.D is unplanned. But it is a mistake to assume that every unplanned pregnancy is unwanted.
So if the tail is still visible at the external os, the I.U.D should be removed. Abortion might occur. If the tail is not at the external os, leave it alone. Abortion might occur or normal pregnancy proceed to term.
The I.U.D will come out with the placenta at the third stage of labour.
In conclusion the author believes that the I.U.D. if properly used is a safe and reliable method of contraception and can prevent unwanted pregnancies and also reduce the number of high risk mothers.
The best people to use I.U.D. are elderly multiparous women who refuse permanent sterilisation.
Author Information
Daw Khin Nyunt
M.B.,B.S(Rgn),FR.C.O.G, Retired Professor Head. Department of Obstetrics and Gynaecology.Institute of Medicine II.Yangon.