Telemedicine for Pediatric Follow-Up Care: A Case Study from Parami General Hospital (PGH), Yangon
I. Introduction
Telemedicine is the use of information and communication technologies to provide healthcare services, which enhances accessibility, affordability, and quality of care. In Myanmar, the COVID-19 pandemic and social unrest have heightened the country’s healthcare needs, particularly in rural areas with limited access to doctors. However, with an internet penetration rate of approximately 90%, telemedicine presents a viable solution. The Golden Zanekka Public Co. Ltd launched a telemedicine project in 2016, offering advanced services through MyanCare, which currently has over 100,000 registered users.
PGH is a prominent center for pediatric healthcare in Myanmar, with many pediatricians working in the emergency, outpatient, and inpatient units. Prof. U Thein Aung is one of the consultants who treat patients at the outpatient department. Typically, some patients who attend the OPD are called for follow-up, with some being asked to attend physical follow-up visits while others attend follow-up sessions online. This decision is based on the patient’s disease condition and place of residence.
During the period between October 2022 and January 2023, Prof. U Thein Aung recommended some pediatric patients to attend their follow-up appointments through teleconsultation. However, due to various reasons, some children were unable to use telemedicine. Only 114 patients attended their follow-up appointments through telemedicine. This case study reports the data for these patients.
II. Objectives
A. General Objective
To develop a telemedicine-supported follow-up and referral system in pediatric practice;
B. Specific Objectives
( a ). To provide telemedicine-based follow-up services to reduce the burden of travel for pediatric patients in remote areas.
( b ). To establish a seamless two-way referral system between consultants in Yangon and doctors in townships.
( c ). To gather data on the savings in terms of traveling time, distance, cost for patients, and patient satisfaction.
III. Operations
Data collection began at the pediatric outpatient department (OPD) at PGH during a physical visit. After being recommended by the consultant for online follow-up, the parents or caregivers were assisted by the MyanCare team in installing and using the application, and some data were collected during that visit.
On the day of the appointment, they attended the teleconsultation session as directed, and some data, such as satisfaction levels and medication prescriptions, were collected during the session. Annexes containing the templates used by the team for collecting quantitative and qualitative data were attached.
The duty of the MyanCare team was to provide IT assistance to both the consultant in Yangon and the patient or GP/specialist at the township. The role of the GP or specialist was to assist the patient in answering the consultant’s questions, perform physical examinations, and report findings to the consultant when necessary. The telemedicine project of GZP participated in data analysis and reporting.
Teleconsultation proceeded as follows:
( a ) The doctor and patient at the township clinic initiated teleconsultations for follow-up appointments by calling the consultant at the hospital (central hub) using MyanCare application.
( b ) Getting the call from the patient/GP, Prof. U Thein Aung at PGH (Yangon), reviewed the patient’s health records, assessed their condition via video, and inquired about their symptoms.
( c ) The local doctor or specialist assisted and reported the findings from the physical examination, including vital signs.
( d ) Based on the findings and reports, the consultant prescribed treatment, recommended investigations, and provided home care guidelines. Patients were encouraged to ask questions, and the system facilitated the delivery of prescribed medication to their homes.
( e ) Finally, the consultant referred the patient back to the local pediatrician or GP.
( f ) The Network Pharmacy Co assisted in obtaining necessary medicines in their respective townships at a reasonable price.
After the teleconsultation session, the MyanCare team asked the mothers for their satisfaction and documented all the data from follow-up and interview. Staff members at Parami Hospital ensured the smooth operation of the process and data transfer between the MyanCare application and Aspire HMIS of PGH.
IV. Results
a. Quantitative data
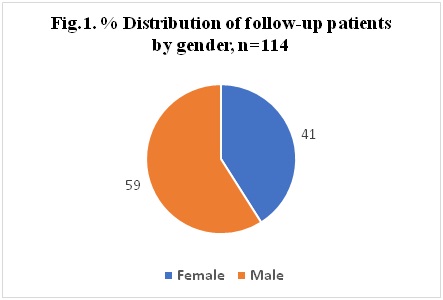
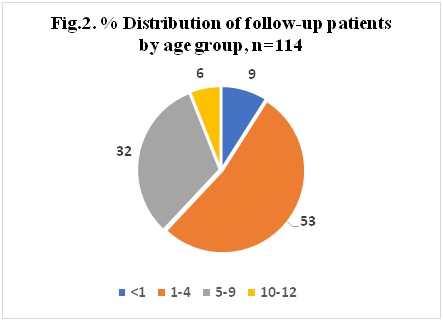
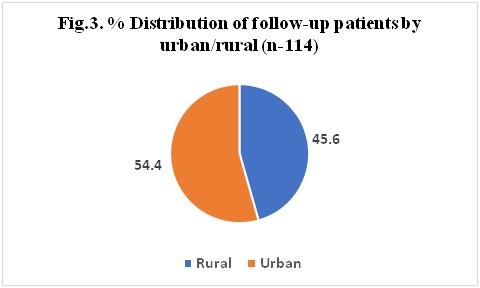
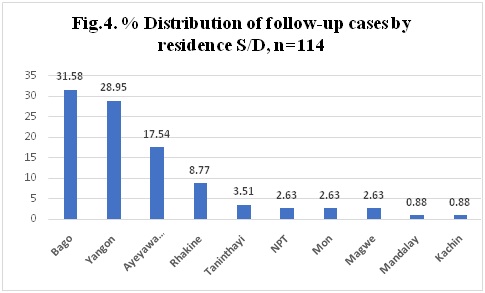
A total of 114 patients were included in this case study. The demographic data showed a female-to-male ratio of 59:41. The highest age group was 1-4 years old. The ratio of urban to rural patients was 54:56, and most of the patients came from Bago, Yangon, and Ayeyarwady divisions.
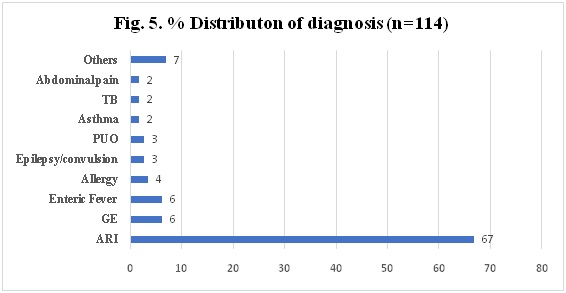
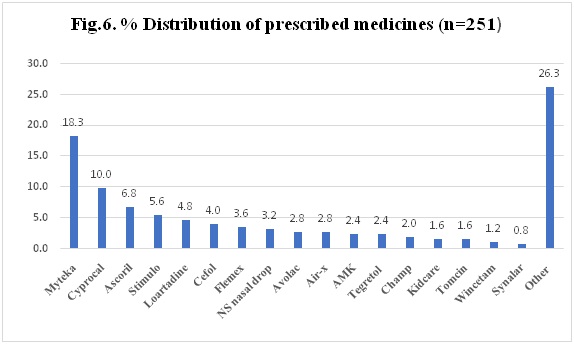
For morbidity, acute respiratory infections (ARI) had the highest incidence rate followed by Gastroenteritis (GE) and Enteric fever (Typhoid). With regards to the individual drug item for medication, Myteka, Cyprocal, and Ascorilwere among the most commonly prescribed drugs for patients with ARI.
Fig.7. Saving for traveling cost, time and distance by telemedicine
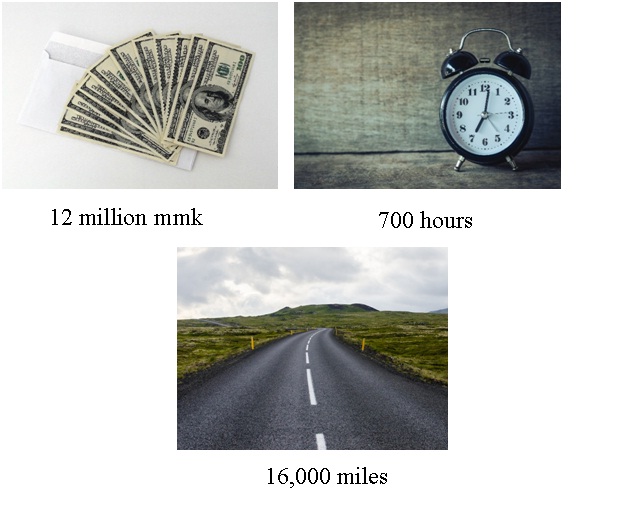
During the 4-month period, the benefits of using telemedicine was demonstrated as 114 follow-up patients were able to save nearly 12 million MMK in travel costs, save around 700 hours in traveling time and avoid traveling approximately 16,000 miles in distance.
8. Waiting time (hours) for medicines
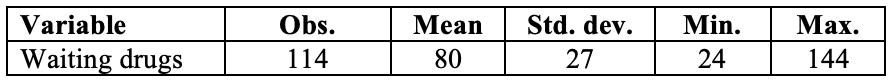
In this case study, the waiting time for the dispensing of one to three prescribed medicines was recorded. The mean time for receiving the medicines was 80 hours, with a standard deviation of 27. An observation was made that 50% of patients received their prescribed medicine within 72 hours after the prescription was made. This metric could provide insight into the efficiency of the medication delivery process and help identify areas for improvement.
b. Qualitative data
During the assessment of mothers’ satisfaction, the MyanCare team interviewed the mother or caretaker using a pretested questionnaire after obtaining a verbal informed consent.
The responses from the mothers indicated that almost all of them were satisfied with the teleconsultation service, but some reported that the connection was weak, making it difficult to hear the consultant’s voice. However, all of them had a positive experience with using teleconsultation for follow-up. Some mothers expressed dissatisfaction with the assistance provided by the local doctor during the consultation.
When asked if they would use telemedicine for their next follow-up, the majority answered “yes,” while approximately 20% responded with “no.” When asked about the reason for this response, they explained that they were more confident with a hands-on examination from the consultant. Nonetheless, they appreciated the benefits of telemedicine in terms of saving time and money for travel.
In this case, one of the BOD members was also interviewed for the view of PGH. In terms of business, he responded that when a patient attended the follow-up appointment online instead of physical visit, the reduced income from hospital was about 9,000 MMK. For this particular case, for 114 follow-up visits, the minimum reduced income from PGH was about 1 million MMK.
V. Discussion
As mentioned earlier, this report was based on routine follow-up sessions conducted by a senior consultant from PGH, and not from a well-designed research study. Therefore, the sample size and sampling method were determined by convenience.
Upon reviewing the data collection form, it was observed that travel costs were considered, but costs for accommodation and meals during physical visits were not accounted for. Regarding the results of the morbidity patterns, the highest diagnosis among children was acute respiratory infection (ARI) followed by GE and Enteric fever, which was in line with the epidemiological pattern observed in developing countries, where infections were the most common cause of illness. It was evident that the demographic and morbidity patterns were not representative of the general population but rather reflected the group of people who typically attend a specialist hospital for day-to-day illnesses.
The benefits of telemedicine was remarkable in terms of the time, money, and travelling saved. Additionally, the reduction in stress associated with avoiding the need to obtain a token and waiting in the OPD should also be considered as a benefit of teleconsultation. While most of the qualitative responses from mothers were positive, it is important to consider the local community’s culture in this context, especially if there is a high potential for Social Desirability Bias. Understanding the cultural norms and values of the community can help in designing effective research methods that minimize the impact of bias and provide more accurate data.
Three parties – the patient, the local doctor (either a general practitioner or specialist), and the consultant from Yangon – participated in telemedicine. It is essential to highlight the benefits that each party derived from this exercise. The patient was able to improve communication with the consultant through the assistance of the local doctor. As a result, they received clarified homecare guidelines, and obtaining prescribed medicines was made easier. The local doctor gained the patient’s trust and confidence, proving to be qualified to work with the consultant from Yangon. Additionally, they had the opportunity to learn from the consultant’s way of thinking and participate in a two-way referral system. The consultant from Yangon received better information about the patient’s symptoms and physical signs with the help of the local doctor. They could also teach their colleague online and ensure the patient’s safety during emergencies, as the local doctor had a good understanding of the patient’s medical history.
Additionally, it is essential to take into account the interests of the hospital management when evaluating the system’s effectiveness on patients. Typically, hospital managers consider the benefits to patients alongside the financial implications for the hospital. This approach can help ensure that the system is sustainable in the long run and can continue to provide quality healthcare services to patients while also meeting the financial goals of the hospital.
In this case study, it was observed that the mean waiting time for medicine was approximately 80 hours with a standard deviation of 27 hours. Waiting for such an extended period could be challenging for patients who are experiencing symptoms of the disease and may impact their recovery and satisfaction.
VI. Recommendations and conclusion:
- MyanCare Co should improve the application for better connection and an improved sound system.
- In considering the effectiveness of teleconsultation, the costs for accommodation, meals, and reduced stress associated with waiting time should also be considered.
- The waiting time for obtaining medicine was observed to be lengthy, and suppliers should explore ways to reduce it.
- Local doctors should be encouraged to participate in the process. Incentives such as a 2-way referral system and on-the-job training should be provided to motivate them.
- In the long-term plan for follow-up visits, the views of the hospital management should be considered, and the benefits for the patients should be emphasized.
- It is important to promote the use of telemedicine for healthcare among both health personnel, especially doctors, and community members. Education should be provided to ensure that individuals understand how to effectively use telemedicine services.
- If feasible, a social research study titled “Assessing the Effectiveness of Teleconsultation among Pediatric Patients” should be conducted to comprehensively evaluate the benefits and limitations of telemedicine for the entire patient population.
Author Information
Kyi Lwin1, Yee Mon2, Hsu Min Aung3, Kaung Mon4, Su Hnin Cho5, Thi Ha Aung6, ZayYar Lwin7, Zaw Min Htun8,Kyaw Thiha9, Kyaw Thin10, Thein Aung11
- Sales Manager, Network Pharmacy.
- Secretary, Telemed Project, GZP.
- Coordinator, MyanCare.
- Team leader, MyanCare.
- Team leader, MyanCare.
- IT Chief, PGH.
- IT Chief, DMH.
- CEO, MyanCare.
- Project Coordinator, GZP.
- Director GZP.
- Professor/consultant of pediatrics, PGH.